Doctors Warn That COVID-19 Infection and Vaccines Triggers Various Dangerous Types of Vasculitis!
Nikhil Prasad Fact checked by:Thailand Medical News Team Dec 10, 2025 1 month, 2 weeks, 2 days, 3 hours, 54 minutes ago
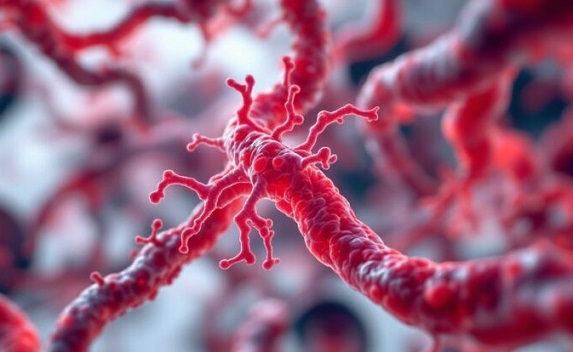
Medical News: In a new in-depth review by researchers from the Kidney Research Center at Tabriz University of Medical Sciences in Iran, evidence shows that both COVID-19 infection and COVID-19 vaccines can lead to the development or worsening of multiple types of vasculitis—a serious condition involving inflammation of the blood vessels. This
Medical News report explores the growing number of clinical cases and mechanisms behind this alarming phenomenon.
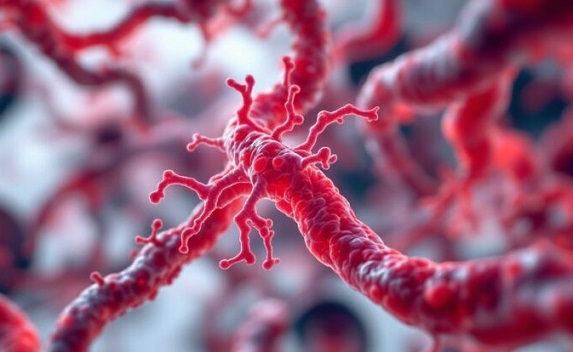 New study shows link between COVID-19 and blood vessel inflammation affecting organs and skin
New study shows link between COVID-19 and blood vessel inflammation affecting organs and skin
The study compiled published case reports, histological evidence, and clinical observations of various forms of vasculitis emerging after either SARS-CoV-2 infection or COVID-19 vaccination.
How COVID and Its Vaccines Cause Blood Vessel Inflammation
The researchers described how SARS-CoV-2 can directly infect blood vessels or indirectly trigger a strong immune response that leads to damage in vessel walls. Mechanisms include immune complex buildup, overactivation of inflammatory pathways, complement system activation, and hypersensitivity reactions. mRNA-based vaccines, particularly Pfizer-BioNTech and Moderna, were more often associated with these reactions compared to other vaccine types.
Some patients developed vasculitis just days after vaccination, while others presented symptoms weeks after COVID-19 infection. In many cases, these were either new (de novo) cases or flare-ups of previously controlled vasculitis.
Symptoms included fever, skin rashes, organ damage, and neurological issues depending on the type of vasculitis.
Vasculitis Types Linked to COVID-19 and Vaccines
The review listed several types of vasculitis that have been observed:
-Urticarial Vasculitis: Skin rashes with immune system overactivation; sometimes appears weeks after COVID-19 recovery.
-Large Vessel Vasculitis (LVV): Inflammation in arteries like the aorta seen in imaging studies; linked to long COVID symptoms.
-ANCA-Associated Vasculitis (AAV): A severe immune attack on small to medium vessels, including kidney and lung involvement. COVID and its vaccines may trigger this by breaking immune tolerance.
-IgA Vasculitis: Often affecting the kidneys and skin, this form was observed in patients with elevated IgA antibodies after COVID-19 or vaccination.
-Cerebral Vasculitis: Inflammation in brain vessels, sometimes causing stroke or hemorrhage. Headache is often the first symptom.
-Leukocytoclastic Vasculitis (LCV): Skin lesions due to small-vessel inflammation, sometimes leading to gangrene or requiring amputations.
-Cutaneous Vasculitis: Appearing
as skin lesions such as purpura, these are linked to both infection and vaccines and can be warning signs of systemic issues.
Cases Linked to COVID-19 Vaccines
Several real-world examples were presented, including:
-A 46-year-old woman with a history of vasculitis who had a flare-up after an mRNA vaccine.
-A 77-year-old man who developed granulomatous vasculitis and acute kidney injury post-AstraZeneca vaccine.
-A 78-year-old woman with past IgA vasculitis who experienced a relapse after vaccination.
-A 31-year-old woman developed severe skin lesions after her second inactivated vaccine dose.
-A 38-year-old man developed small-vessel vasculitis resulting in a brain hemorrhage.
Notably, some patients experienced only mild skin reactions, while others faced severe complications like kidney failure, gangrene, or brain inflammation.
A Rare Yet Real Risk That Needs Monitoring
Though vasculitis following COVID-19 vaccination is rare, the study emphasizes that it should not be ignored—especially in individuals with prior autoimmune conditions. Healthcare providers are urged to monitor for symptoms of vasculitis after vaccination or infection. Early intervention with corticosteroids or immunosuppressive therapies can reduce damage and improve recovery.
Understanding these mechanisms could help guide better screening, vaccine strategies, and post-infection care—especially for vulnerable groups.
The study findings were published in the peer reviewed Virology Journal.
https://link.springer.com/article/10.1186/s12985-025-03032-x
For the latest COVID-19 News, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/articles/coronavirus
https://www.thailandmedical.news/articles/long-covid
https://www.thailandmedical.news/articles/vaccine-news