Natural Killer Cells Reveal Why Some Omicron COVID Cases Stay Mild While Others Worsen
Nikhil Prasad Fact checked by:Thailand Medical News Team May 13, 2025 9 months, 6 days, 10 hours, 26 minutes ago
Medical News: Natural Killer Cells Hold the Key to Understanding Why Omicron Affects People So Differently
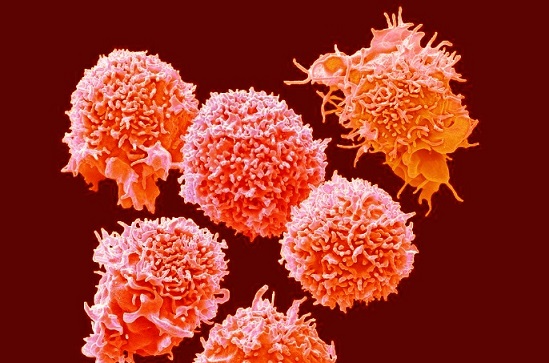
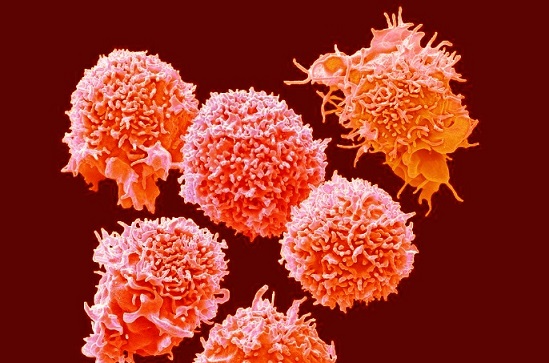
A new Japanese study has found that the body’s natural killer (NK) cells—special immune cells that help fight off viruses—respond very differently in mild versus moderate cases of COVID-19 caused by the Omicron variant. These differences could help explain why some people recover quickly, while others need hospital care despite being infected with what is considered a “milder” strain.
 Natural Killer Cells Reveal Why Some Omicron COVID Cases Stay Mild While Others Worsen
Natural Killer Cells Reveal Why Some Omicron COVID Cases Stay Mild While Others Worsen
The research was conducted by scientists from multiple divisions within Tottori University in Japan, including the Division of Infectious Diseases, the Department of Multidisciplinary Internal Medicine, and the Department of Pathobiological Science and Technology. This
Medical News report covers their discoveries in detail, revealing how subtle shifts in immune activity may shape a patient’s entire illness trajectory.
Mild Cases Show Unusual NK Cell Activation Without Full Immune Attack
In the study, researchers followed 27 COVID-19 patients hospitalized between January and May 2022, during the peak of the Omicron wave in Japan. These patients were classified as having either mild or moderate COVID-19 based on national medical guidelines. Blood samples were collected at different stages of illness to examine how NK cells were behaving.
In mild cases, the researchers found a specific subtype of NK cells—called CD56dimCD16- NK cells—was more active. These cells had higher levels of an “activating” protein called NKG2D, which normally signals NK cells to attack infected cells. However, despite this activation signal, the NK cells in mild cases released much fewer toxic substances such as granzyme A, granzyme B, and granulysin, which are typically used to destroy virus-infected cells. This suggests the immune system was prepared to fight but held back, possibly avoiding unnecessary inflammation.
Moderate Cases Show Signs of Immune Burnout and Inflammation
In contrast, moderate COVID-19 cases showed what scientists call “immune exhaustion.” The NK cells in these patients had much higher levels of TIGIT, a marker that signals the immune cells to stop fighting. Despite the presence of activating signals, these NK cells seemed burnt out and ineffective. This may be due to prolonged stimulation by viral proteins and inflammatory substances in the body.
Moreover, blood tests revealed that patients with moderate COVID-19 had much higher levels of inflammatory cytokines—chemical messengers like IL-6, TNF-alpha, and interferons that are involved in causing fever, inflammation, and fatigue. A molecule called sULBP2 was also found in significantly greater quantities in these patients. sULBP2 is a marker that reflects immune system activation and is typically found in greater amounts when the body is fighting a strong viral infection.
r />
The researchers used advanced statistical methods, including principal component analysis, to map out how these immune markers interact. They found that sULBP2 was closely linked with other inflammatory markers, suggesting it could serve as a warning sign for when a mild case might progress into something more serious.
Why These Findings Matter
These insights are critical in the Omicron era, where most cases are classified as mild or moderate. Understanding the differences in immune responses—especially the behavior of NK cells—can help doctors predict who might get worse and need closer monitoring or early treatment.
The study also provides clues for future treatments. If scientists can find ways to prevent NK cell exhaustion or fine-tune their activity, they might be able to keep moderate cases from escalating. Similarly, if sULBP2 is confirmed as a reliable marker of immune overactivation, it could be used as a simple blood test to detect high-risk patients early.
Study Conclusions
This study shows that the body’s first line of defense against COVID-19—the natural killer cells—respond very differently based on the severity of illness. In mild Omicron cases, the NK cells are active but restrained, possibly to prevent unnecessary inflammation. In moderate cases, however, these cells become overstimulated and exhausted, losing their ability to fight the virus effectively.
This imbalance is accompanied by a rise in dangerous inflammatory substances and immune markers like sULBP2 and IL-6. Understanding these mechanisms may help identify those at risk of worsening illness and offer new therapeutic targets. The findings also emphasize the importance of early immune monitoring even in seemingly mild cases of COVID-19.
The study findings were published in the peer reviewed journal: Frontiers in Immunology.
https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1594296/full
For the latest COVID-19 News, keep on logging to Thailand Medical News.
Read Also:
https://www.thailandmedical.news/news/new-study-links-long-covid-to-reduced-natural-killer-cell-activity
https://www.thailandmedical.news/news/new-mutation-emerges-in-sars-cov-2-nsp13-protein-that-allows-escape-from-nk-cell-recognition
https://www.thailandmedical.news/news/breaking-medical-news-italian-study-shows-that-covid-19-vaccines-causes-persistent-cd16-downmodulation-and-nk-cell-impairment
https://www.thailandmedical.news/articles/coronavirus
https://www.thailandmedical.news/pages/thailand_doctors_listings