Doctors Warn That COVID-19 Infections Can Trigger Dangerous Brain Syndrome in Individuals on Antipsychotic Medications
Nikhil Prasad Fact checked by:Thailand Medical News Team Jun 01, 2025 8 months, 3 weeks, 3 days, 1 hour, 30 minutes ago
Thailand Medical News: A new case report from researchers at the University Hospital in Ostrava, Czech Republic, has highlighted a dangerous medical complication that may arise in individuals with psychiatric disorders who contract COVID-19. The condition in question is Neuroleptic Malignant Syndrome (NMS), a rare but potentially fatal reaction to antipsychotic medications. According to the researchers, SARS-CoV-2—the virus responsible for COVID-19—might play a more active role in triggering or exacerbating this condition than previously thought.
 Doctors Warn That COVID-19 Infections Can Trigger Dangerous Brain Syndrome in Individuals on Antipsychotic Medications
Doctors Warn That COVID-19 Infections Can Trigger Dangerous Brain Syndrome in Individuals on Antipsychotic Medications
The research was conducted by Tomas Skront and Martin Hyza from the Department of Psychiatry, and Jiri Sagan from the Department of Infectious Diseases, all at the University Hospital in Ostrava, Czech Republic. Their case study and review of previous reports serve as a stark warning to clinicians worldwide. This
Thailand Medical News report provides an in-depth breakdown of the findings and what they could mean for future patient care.
What Is Neuroleptic Malignant Syndrome
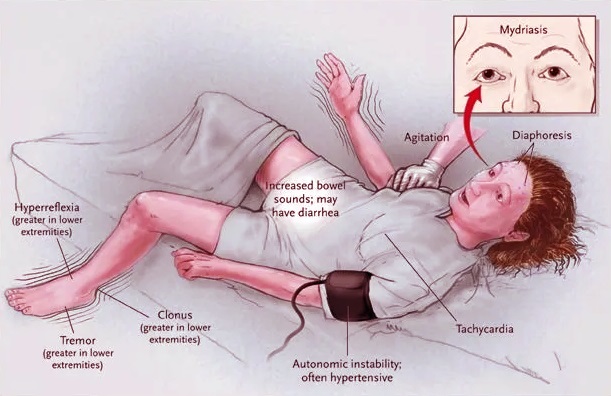
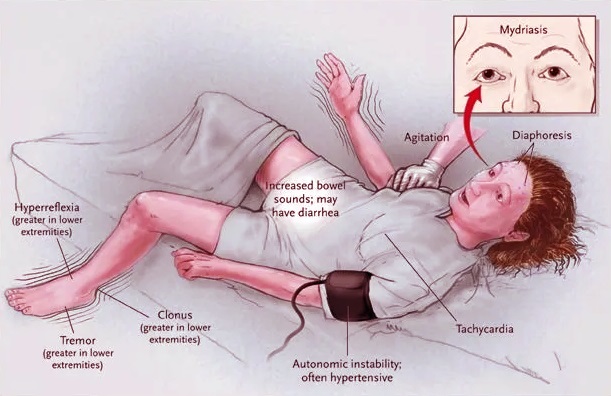
NMS is a life-threatening condition typically associated with the use of dopamine-blocking antipsychotic medications. It is characterized by high fever, muscle rigidity, altered mental status, and autonomic dysfunction (such as unstable blood pressure and heart rate). While NMS is rare, it is well-documented among patients on medications like haloperidol, olanzapine, clozapine, and risperidone.
What makes this new case so alarming is that the syndrome appeared in a young man during the course of a COVID-19 infection—and the authors suggest that the virus may have played a key role in making him more vulnerable.
Case Details a Complex Cascade
The subject of the case was a 29-year-old male with a history of treatment-resistant schizophrenia. He had been stable on long-term treatment that included paliperidone, clozapine, and cariprazine. He was brought to the emergency department in an aggressive, confused state and was later confirmed to have COVID-19.
Soon after admission, he experienced a serious respiratory crisis and required intubation. He also developed pneumonia, and his medication regimen was modified to include high doses of olanzapine and later haloperidol. Within days of the new antipsychotic additions, he began showing signs of NMS—fever, muscle rigidity, mental confusion, excessive sweating, and elevated creatine kinase levels, a marker of muscle damage.
How COVID May Set the Stage for NMS
SARS-CoV-2 is known to bind to ACE2 receptors, which are found in the lungs and many other tissues—including the brain. These receptors are co-expressed with DOPA decarboxylase (DDC), an enzyme vital for dopamine and serotonin synthesis. COVID-19 can downregulate both ACE2 and DDC, potentially disturbing the delicate balance of neurotransmitters in the brain.
In people with schizophrenia—already prone to dopamine imbalances—this viral interference could tip the scale, especially when antipsychotic medications further reduce dopamine signaling. The case raises the possibility that SARS-CoV-2 infection may amplify the brain’s vulnerability to antipsychotic toxicity and trigger NMS even at doses that might otherwise be well-tolerated.
Not Just One Case A Pattern Emerges
The Ostrava researchers also reviewed 11 other cases of NMS that occurred in the context of COVID-19 infection or shortly after COVID-19 vaccination. These cases included individuals with schizophrenia, epilepsy, bipolar disorder, and even no psychiatric history at all.
Some patients were already on antipsychotics; others received these drugs during hospitalization for COVID-19 complications. In a few cases, NMS occurred in individuals following COVID-19 vaccination. Although causality is hard to prove, these occurrences point to an unsettling overlap between SARS-CoV-2 exposure, immune response, and neuropsychiatric medication side effects.
In all cases, symptoms were consistent with classic NMS: hyperthermia, muscle stiffness, altered consciousness, and lab abnormalities. Most patients survived with treatment, which often involved the dopamine agonist bromocriptine and muscle relaxants like dantrolene, but at least two patients died despite intervention.
Key Observations from The Case
In the featured case, the young patient’s condition deteriorated rapidly following multiple injections of haloperidol, a first-generation antipsychotic known for its strong dopamine-blocking action. His fever remained high despite antipyretics, his CK levels surged to 21 µkat/L (normal upper limit is 2.85 µkat/L), and he showed signs of extreme autonomic instability.
Once haloperidol and olanzapine were discontinued and bromocriptine plus clonazepam therapy was initiated, his symptoms gradually subsided. He was eventually stabilized on clozapine alone and discharged after 52 days in the hospital.
What Doctors Should Take Away
This case and the reviewed literature should make clinicians more cautious when managing psychiatric patients who are infected with COVID-19. Inflammatory cytokines released during infection may interfere with drug metabolism (especially via liver enzymes like CYP3A4 and CYP2D6), leading to higher drug levels and toxicity. COVID-19 may also directly affect the central nervous system and alter neurotransmitter dynamics.
Given these risks, healthcare providers should consider:
-Avoiding sudden increases in antipsychotic dosing during active infection
-Monitoring for early signs of NMS in psychiatric and ICU patients alike
-Using second-generation antipsychotics with greater caution
-Avoiding polypharmacy when possible, especially during COVID-related hospitalization
-Evaluating alternatives to sedation when managing agitation in COVID patients
Conclusions
The findings suggest that COVID-19 is not just a respiratory illness—it may also act as a neurological and psychiatric destabilizer in vulnerable individuals. Its ability to disrupt dopamine and serotonin pathways through ACE2 and DDC interactions, as well as its impact on inflammation and metabolism, could predispose certain patients to life-threatening drug reactions like neuroleptic malignant syndrome.
The case presented by the Czech team, along with their detailed review of previous incidents, underscores the need for vigilance. While rare, NMS is deadly when unrecognized and can complicate both psychiatric care and COVID-19 management. Clinicians must be aware of the broader neurological impact of SARS-CoV-2, especially in patients on neuroactive medications.
This case also raises important questions about the interplay between infection, immunity, and psychiatric pharmacology. With more emerging viruses and novel vaccines on the horizon, understanding these complex interactions will be crucial. More retrospective studies and pharmacovigilance reports are needed to determine how common these interactions are and what protocols can be put in place to mitigate them.
The study findings were published in the peer reviewed journal: BMC Psychiatry
https://link.springer.com/article/10.1186/s12888-025-07032-7
For the latest COVID-19 News, keep on logging to
Thailand Medical News.
Read Also:
https://www.thailandmedical.news/news/covid-19-alters-drug-effects-through-cyp3a4-enzyme-dysregulation
https://www.thailandmedical.news/news/breaking-a-must-for-all-doctors-to-read-scientists-warn-that-covid-19-affects-cytochrome-p450-3a4-mediated-drug-metabolism-and-drug-interactions
https://www.thailandmedical.news/news/covid-19-inhibits-cytochrome-p450-enzymes-that-metabolize-drugs-like-antipsychotics-leading-to-higher-blood-levels
https://www.thailandmedical.news/articles/coronavirus
https://www.thailandmedical.news/articles/coronavirus