Nikhil Prasad Fact checked by:Thailand Medical News Team Nov 29, 2024 1 year, 2 months, 2 weeks, 21 hours, 40 minutes ago
Medical News: The Connection Between Tuberculosis and Diabetes
Recent research highlights a concerning link between type 2 diabetes (T2D) and tuberculosis (TB), revealing how diabetes impairs the immune system's ability to combat TB. A collaborative study involving experts from institutions such as Stellenbosch University, University of Cape Town, Mater Research Institute at the University of Queensland, and Texas Biomedical Research Institute explores these findings. The study delves into the role of alveolar macrophages - lung immune cells crucial for fighting TB - and how their function is affected by diabetes.
 Tuberculosis Risk Increases in Diabetes Patients
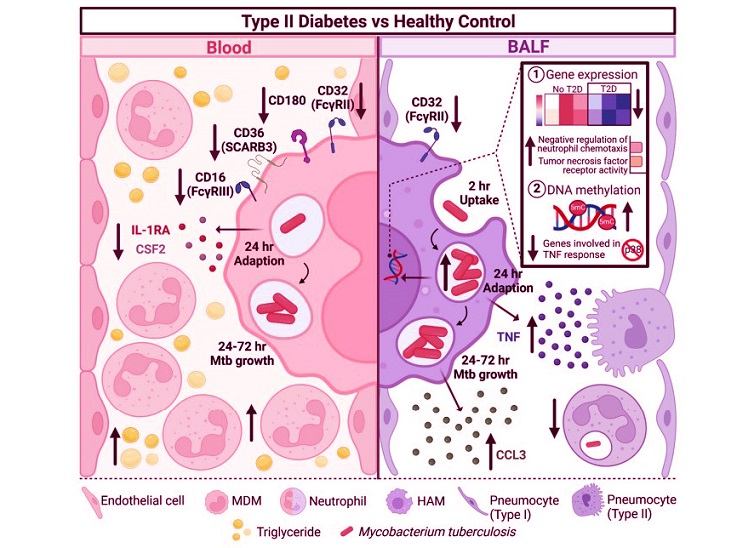
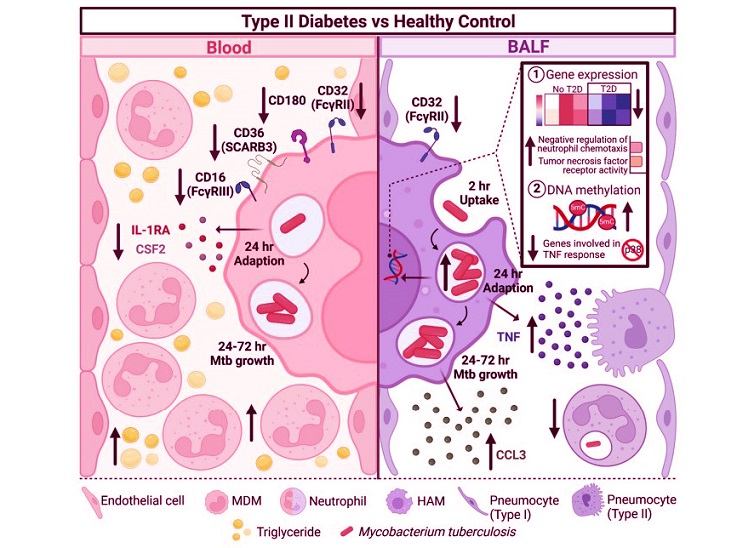
Schematic summary of differences in the response of human monocyte-derived macrophage (MDM) and alveolar macrophage (HAM) to Mtb, by type 2 diabetes status. The blood of T2D patients has higher levels of glucose and triglycerides and circulating white blood cells and neutrophil counts. In contrast, T2D patients have lower neutrophil percentages in their bronchoalveolar lavage fluid. MDMs from T2D patients express less CD32, CD180, CD36 and CD16 and produce less IL-1RA and CSF2 (GM-CSF) in response to M.tb infection (day 1 p.i.). However, these changes did not result in changes in the ability of MDMs to phagocytose or kill M.tb. HAMs from T2D patients also express less CD32. HAMs, however, produce more TNF (day 1 p.i.) and CCL3 (MIP-1α) (day 3 p.i.) in response to M.tb. Twenty-four h (day 1) p.i., HAMs of T2D patients have a significantly higher bacterial burden which coincides with an overall decrease in gene expression and increase in DNA methylation.
Tuberculosis Risk Increases in Diabetes Patients
Schematic summary of differences in the response of human monocyte-derived macrophage (MDM) and alveolar macrophage (HAM) to Mtb, by type 2 diabetes status. The blood of T2D patients has higher levels of glucose and triglycerides and circulating white blood cells and neutrophil counts. In contrast, T2D patients have lower neutrophil percentages in their bronchoalveolar lavage fluid. MDMs from T2D patients express less CD32, CD180, CD36 and CD16 and produce less IL-1RA and CSF2 (GM-CSF) in response to M.tb infection (day 1 p.i.). However, these changes did not result in changes in the ability of MDMs to phagocytose or kill M.tb. HAMs from T2D patients also express less CD32. HAMs, however, produce more TNF (day 1 p.i.) and CCL3 (MIP-1α) (day 3 p.i.) in response to M.tb. Twenty-four h (day 1) p.i., HAMs of T2D patients have a significantly higher bacterial burden which coincides with an overall decrease in gene expression and increase in DNA methylation.
This
Medical News report delves into how T2D influences immune responses, particularly at the site of TB infection, the lungs. These findings not only enhance understanding of TB susceptibility but also provide insights into immune dysfunction in diabetes patients.
Key Findings of the Study
Alveolar macrophages, the first line of defense against TB, showed reduced ability to control Mycobacterium tuberculosis (M.tb) in diabetes patients. Researchers discovered that these cells were less effective in containing TB bacteria in the initial stages of infection. This dysfunction was linked to various factors, including altered immune signaling, delayed gene expression, and DNA methylation changes in the macrophages.
The study also found that diabetes patients had lower levels of neutrophils in their lung fluid. Neutrophils are essential immune cells that work alongside macrophages to eliminate TB bacteria. Reduced neutrophil presence was directly correlated with higher bacterial growth in alveolar macrophages. This highlights the critical role of macrophage-neutrophil interactions in maintaining lung immunity.
Insights Into Gene Expression and Cytokine Responses
Researchers noted that gene expression in alveolar macrophages of diabetes patients was delayed. While normal cells ramped up immune responses quickly a
fter TB infection, those from diabetes patients exhibited sluggish activation. Genes involved in regulating neutrophil movement and tumor necrosis factor (TNF) signaling were particularly affected.
Moreover, the study revealed heightened TNF production by macrophages in diabetes patients. While TNF plays a crucial role in controlling TB, excessive levels can lead to lung tissue damage and worsen TB outcomes. This imbalance may contribute to the severe disease progression seen in diabetes patients.
DNA Methylation and Immune Dysregulation
An intriguing finding was the increased DNA methylation in lung cells of diabetes patients, which impacted genes linked to immune function. For instance, genes involved in TNF response and neutrophil regulation were hypomethylated, correlating with abnormal cytokine production. This epigenetic change provides a molecular explanation for the impaired immune responses in diabetes patients.
The study also compared immune responses between alveolar macrophages and monocyte-derived macrophages (MDMs). While MDMs from diabetes patients showed reduced production of certain immune factors, they were less affected than alveolar macrophages, underscoring the unique challenges faced by lung-specific immune cells.
Broader Implications of the Findings
This research offers crucial insights into why diabetes patients are more susceptible to TB. By identifying specific immune deficiencies - such as reduced neutrophil recruitment, delayed gene activation, and altered cytokine responses - the study paves the way for targeted interventions. Enhancing lung immunity in diabetes patients could significantly reduce TB risk and improve treatment outcomes.
Furthermore, the findings emphasize the need for integrating TB and diabetes management in healthcare policies, particularly in regions with high burdens of both diseases. Strategies such as better blood sugar control and early TB screening for diabetes patients could help mitigate the dual epidemic.
Study Limitations and Future Directions
While the study provides valuable insights, researchers acknowledge its limitations, including a small sample size and focus on a single geographic region. Future studies involving larger, diverse populations could validate and expand upon these findings. Exploring therapeutic approaches to modulate immune responses and epigenetic changes in diabetes patients may also hold promise.
Conclusion
The research underscores the profound impact of type 2 diabetes on lung immunity, revealing mechanisms that increase TB susceptibility. Alveolar macrophages in diabetes patients are less effective in combating TB bacteria due to delayed immune activation, altered cytokine production, and reduced neutrophil recruitment. These findings highlight the need for a comprehensive approach to TB prevention and treatment in diabetes patients, integrating medical, immunological, and policy perspectives.
The study findings were published on a preprint server and are currently being peer reviewed.
https://www.researchsquare.com/article/rs-5489046/v1
For the latest TB News, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/new-strategies-for-combating-tuberculosis-with-repurposed-drugs-and-natural-remedies
https://www.thailandmedical.news/news/scientists-anticipate-that-tuberculosis-will-the-next-global-health-crisis-as-new-antibiotic-resistance-genes-have-been-identified
https://www.thailandmedical.news/articles/tuberculosis-tb-news