Nikhil Prasad Fact checked by:Thailand Medical News Team Nov 09, 2024 1 year, 3 months, 2 weeks, 20 hours, 29 minutes ago
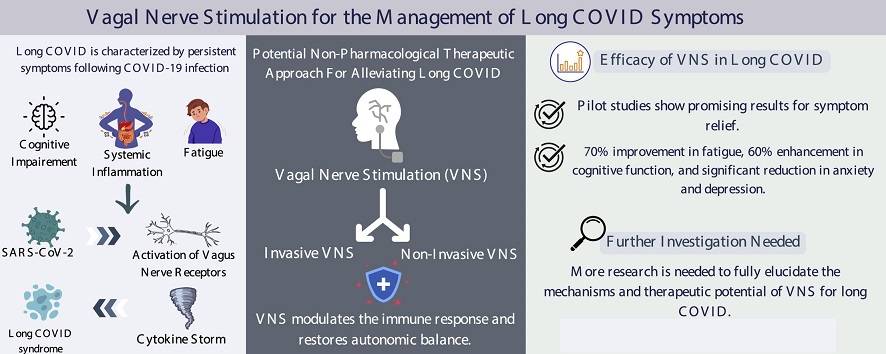
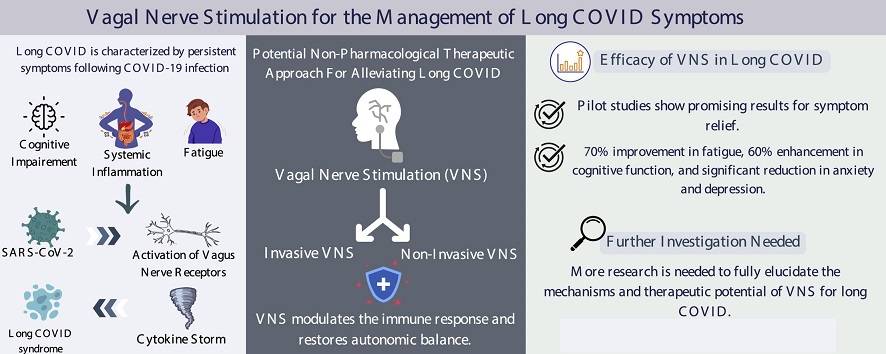
Medical News: Researchers from Yale University-USA, Khyber Medical College, and the Cleveland Clinic-USA have turned their attention to a novel method called vagus nerve stimulation (VNS) to alleviate persistent symptoms associated with long COVID. This new approach, non-invasive and generally well-tolerated, is gaining traction as a way to help those who continue to suffer even months after initial infection. This
Medical News report dives into how vagus nerve stimulation (VNS) may provide a safe and effective option for those seeking relief from the lingering effects of COVID-19.
 Vagus Nerve Stimulation as a New Hope for Long COVID Relief
Vagus Nerve Stimulation as a New Hope for Long COVID Relief
Long COVID, a condition experienced by individuals who continue to face symptoms well after recovery from COVID-19, has left countless patients struggling with fatigue, cognitive impairments, and autonomic dysfunction. The vagus nerve, central to controlling inflammation and maintaining the body's internal balance, could be a key player in easing these symptoms through VNS.
The Role of the Vagus Nerve in Long COVID
The vagus nerve, a crucial component of the body’s autonomic nervous system, influences heart rate, digestion, and immune response. COVID-19’s impact often leads to a “cytokine storm” - an aggressive inflammatory response that disrupts the body's balance and triggers symptoms like fatigue, mental fog, and shortness of breath. The prolonged immune activation in long COVID may also create persistent neurological issues. Studies highlight that patients with ongoing symptoms after COVID-19 show abnormal inflammatory markers that are not present in recovered, asymptomatic individuals. This prolonged inflammation is believed to interfere with normal vagus nerve functioning, potentially explaining some of the cognitive and physical symptoms seen in long COVID.
VNS, which stimulates the vagus nerve, may help to dampen this prolonged immune response. By activating the cholinergic anti-inflammatory pathway (CAP), VNS can potentially reset the autonomic balance, reduce inflammation, and relieve symptoms such as fatigue and cognitive impairment, which are common among long COVID patients.
Types of Vagus Nerve Stimulation and How They Work
VNS is available in two primary forms: invasive and non-invasive. Invasive VNS involves surgically implanted devices that deliver electrical impulses directly to the vagus nerve. However, non-invasive VNS (nVNS), such as transcutaneous auricular VNS (taVNS) or transcutaneous cervical VNS (tcVNS), is easier to administer and does not require surgery, making it a promising approach for long COVID patients.
-Auricular VNS (taVNS): In this method, a device stimulates the vagus nerve through the ear, targeting specific areas to produce anti-inflammatory effects.
-Cervical VNS (tcVNS): This approach targets the vagus nerve via the neck and has shown potential benefits in managing depression, anxiety, and fatigue - conditions often observed in long COVI
D patients.
The versatility of these methods allows individuals to potentially use nVNS at home with devices designed for personal use. This convenient approach has sparked interest in further studies and clinical trials to evaluate its effectiveness in managing long COVID symptoms.
Key Findings and Initial Success with VNS in Long COVID
Preliminary studies on vagus nerve stimulation (VNS) for long COVID indicate promising outcomes, with improvements noted in various cognitive, respiratory, and physical symptoms. A recent study involving female long COVID patients showed significant improvement in cognitive function, anxiety, depression, and sleep after 10 days of using tcVNS. These findings align with earlier research that suggests VNS can restore autonomic balance, potentially addressing the root of long COVID's lingering effects.
In another pilot trial conducted in Spain, researchers found that nVNS helped lower inflammation levels, particularly procalcitonin and C-reactive protein (CRP) levels. Elevated levels of these biomarkers have been associated with poor COVID-19 outcomes, so a reduction could signal improved patient responses to nVNS therapy.
Other studies have shown positive outcomes using taVNS to address cognitive and emotional symptoms in long COVID patients. By reducing systemic inflammation and promoting normal brain function, taVNS may be especially helpful in treating neurological symptoms associated with the condition. Notably, in an open-label pilot study, 12 patients self-administered taVNS safely, with eight out of 14 participants showing notable improvements in fatigue and mental clarity.
Mechanisms Behind VNS and Its Impact on Inflammation
Vagus nerve stimulation (VNS) is believed to help modulate the body’s inflammatory response by stimulating the CAP pathway. This mechanism influences the production of pro-inflammatory cytokines like IL-6 and TNF-α, which are often elevated in long COVID patients and linked to many of the condition’s persistent symptoms. Research suggests that by lowering these inflammatory cytokines, VNS may reduce the impact of inflammation on the body, alleviating symptoms like brain fog and fatigue.
In addition to reducing inflammation, vagus nerve stimulation affects neurotransmitter levels, which can help stabilize mood and cognitive function. This effect has been seen in treating conditions like depression and anxiety, where VNS improved overall mental well-being. These cognitive and emotional benefits may explain why vagus nerve stimulation has shown potential in treating long COVID, as patients commonly report struggles with memory, focus, and mood stability.
Safety and Tolerance of VNS in Long COVID
Non-invasive vagus nerve stimulation (VNS) has proven to be safe with minimal side effects, making it a viable option for those dealing with long COVID. According to a comprehensive review involving over 1,300 participants, common side effects are mild and include skin irritation, headache, and occasional hoarseness. The dropout rate due to side effects was very low, suggesting that taVNS is generally well-tolerated.
In comparison, invasive VNS has more potential complications due to surgical requirements, including infection and vocal cord issues. However, for many patients, the potential relief from chronic symptoms may outweigh these risks, especially when considering the low-risk profile of non-invasive VNS options.
Limitations and the Need for Further Research
Although the initial findings are promising, the evidence supporting vagus nerve stimulation for long COVID remains limited. Most studies are small-scale pilot trials, and larger, controlled studies are necessary to determine the therapy’s long-term effectiveness and safety. The need for standardized protocols and a clearer understanding of VNS’s mechanisms in reducing long COVID symptoms is vital to advancing its clinical use.
There is also a need for studies examining how vagus nerve stimulation impacts different demographics within the long COVID population. Gender, age, and pre-existing health conditions may influence the therapy's effectiveness. Understanding these variables could allow for more targeted, personalized applications of VNS, aligning with the broader goals of precision medicine.
Conclusion: A Promising Future for Vagus Nerve Stimulation in Long COVID Treatment
The use of vagus nerve stimulation as a potential therapy for long COVID represents a promising new approach in managing this complex condition. With its ability to restore autonomic balance, reduce inflammation, and improve mental health, vagus nerve stimulation may offer relief for patients who have struggled to find effective treatments. Although further research is needed to confirm these findings on a larger scale, early results suggest that non-invasive VNS could play a significant role in addressing the persistent symptoms of long COVID.
As scientific understanding deepens, vagus nerve stimulation may become a staple in the management of long COVID and potentially other post-viral syndromes. Researchers are optimistic that with continued study, this innovative therapy could offer patients a path to recovery and a return to normal life. For now, those interested in this therapy should consult with medical professionals to explore its suitability.
The study findings were published in the peer-reviewed journal: Infectious Medicine.
https://www.sciencedirect.com/science/article/pii/S2772431X24000637
For the latest on Long COVID, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/study-finds-that-home-based-transcutaneous-auricular-vagus-nerve-stimulation-tavns-therapy-can-help-in-long-covid
https://www.thailandmedical.news/news/tens-therapy-shows-promise-for-long-covid-pain-relief
https://www.thailandmedical.news/news/spanish-researchers-claim-sars-cov-2-causes-dysfunction-of-vagus-nerve,-resulting-in-a-variety-of-conditions-associated-with-long-covid
https://www.thailandmedical.news/news/spanish-study-reveals-the-role-of-vagus-nerve-dysfunction-caused-by-sars-cov-2-in-post-covid-19-conditions