COVID-19 News: Physicians Warn That SARS-CoV-2 Infections Can Also Lead To Hypophysitis Based On A Case Study
Nikhil Prasad Fact checked by:Thailand Medical News Team Oct 20, 2023 2 years, 3 months, 4 weeks, 2 days, 15 hours, 35 minutes ago
COVID-19 News: In the wake of the COVID-19 pandemic, an increasing number of patients are reporting a wide range of complications and lingering symptoms that extend beyond respiratory issues. Recently, medical professionals have issued a warning about a rare condition known as hypophysitis, which involves inflammation of the pituitary gland. This article will explore the connection between COVID-19 and hypophysitis, drawing attention to a case study and its implications.
Already past
COVID-19 News reports have shown that SARS-CoV-2 is able to infect the pituitary gland and also cause various issues.
https://www.thailandmedical.news/news/breaking-news-italian-study-reveals-that-sars-cov-2-is-able-to-affect-the-pituitary-gland-leading-to-possible-hypopituitarism-and-a-variety-of-disorde
https://www.thailandmedical.news/news/thailand-medical-news-warns-that-covid-19-infections-and-covid-19-vaccines-can-cause-pituitary-apoplexy-and-possibly-pituitary-adenomas
Hypophysitis: A Multifaceted Condition
Hypophysitis is a condition characterized by inflammation of the pituitary gland, which can be primary or secondary to various local or systemic processes. The diagnosis of hypophysitis is often challenging due to its wide differential diagnosis, which includes primary tumors, metastases, lymphoproliferative diseases, and autoimmune causes. Patients with hypophysitis typically present with headaches, anterior and/or posterior pituitary dysfunction, and imaging evidence of pituitary gland enlargement or stalk thickening. While autoimmune factors are the primary cause, hypophysitis can also result from inflammation due to sellar tumors or cysts, systemic diseases, infection, or drug-induced factors.
Emerging subtypes of hypophysitis, such as immunoglobulin G4-related hypophysitis, immunotherapy-induced hypophysitis, and paraneoplastic pituitary-directed autoimmunity, further complicate the landscape of this rare pituitary condition.
Accurate diagnosis often requires a pituitary biopsy, but in many cases, a presumptive diagnosis is made based on clinical history and examination, with imaging playing a supplementary role. Treatment strategies vary but may include hormone replacement, glucocorticoids to reduce mass effect, and, in some cases, surgery, immunosuppressive therapy, or radiation therapy.
COVID-19 and Its Impact on the Pituitary Gland
COVID-19, caused by the SARS-CoV-2 virus, has demonstrated a multifaceted impact on the human body. The virus primarily enters host cells through the interaction of the spike (S) protein with angiotensin-converting enzyme 2 (ACE2) receptors. These ACE2 receptors are not limited to the respiratory system; they are found in various human tissues and organs, including the heart, lung, kidne
y, testis, and even the brain. This broad distribution of ACE2 receptors may explain the diverse and widespread symptoms seen in COVID-19 patients.
While the predominant symptoms of COVID-19 are respiratory in nature, the moderate expression of ACE2 in other organs, including endocrine glands such as the pituitary, has raised concerns about potential effects on these organs. Until recently, direct damage to the pituitary gland following a COVID-19 infection was scarcely reported in the medical literature.
A Case Study: COVID-19 and Hypophysitis
This rare connection between COVID-19 and hypophysitis became evident in a case involving a 31-year-old healthy athlete as reported by doctors and researchers from University of Puerto Rico School of Medicine, San Juan- USA. She had no prior systemic illness but experienced an array of symptoms after contracting COVID-19, including hypotension, symptomatic hypoglycemia, and a loss of appetite. Additionally, her postpartum state was complicated by the absence of menstruation and the inability to lactate, both of which emerged following her COVID-19 infection. Laboratory investigations revealed pancytopenia, sustained hypoglycemia, and central adrenal insufficiency.
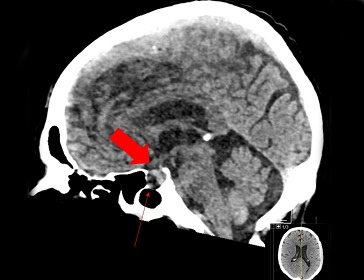
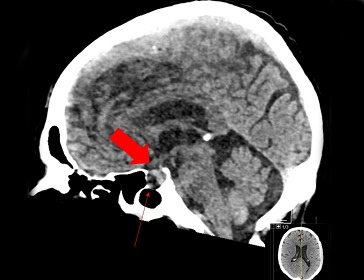
Further assessments unveiled secondary hypothyroidism and imaging evidence of pituitary gland enlargement and stalk thickening. A presumptive diagnosis of hypophysitis was made, leading to the initiation of corticosteroid therapy. While her hypoglycemia, hypotension, and anorexia resolved with treatment, diabetes insipidus emerged.
The patient was ultimately diagnosed with panhypopituitarism, which encompassed hypogonadotropic hypogonadism, hypoprolactinemia, and growth hormone deficiency. This unique case highlights panhypopituitarism as a rare consequence of COVID-19 and underscores the importance of considering endocrinopathies in post-COVID-19 patients with persistent non-specific symptoms.
Implications and Conclusion
The connection between COVID-19 and hypophysitis, as demonstrated by this case study, highlights the need for vigilance among healthcare providers. In patients with lingering, non-specific symptoms following a COVID-19 infection, a high index of suspicion for endocrinopathies, such as hypophysitis, is crucial. Early recognition and intervention can lead to improved outcomes and a better quality of life for affected individuals.
As we continue to navigate the evolving landscape of the COVID-19 pandemic, it is essential to explore and understand its potential impacts on various organ systems. Hypophysitis is just one example of the many health challenges that may arise in the wake of this novel virus. By staying informed and vigilant, the medical community can adapt to the ever-changing circumstances and provide the best possible care to patients affected by COVID-19 and its associated complications.
The case report was published as an abstract in the peer reviewed Journal of the Endocrine Society.
https://academic.oup.com/jes/article/7/Supplement_1/bvad114.1264/7290890
For the latest
COVID-19 News, keep on logging to Thailand Medical News.