COVID-19 News: More Case Reports Emerging Of COVID-19 Patients Manifesting Pneumomediastinum Or Mediastinal Emphysema!
COVID-19 News - Pneumomediastinum Jan 11, 2023 3 years, 1 month, 1 week, 5 days, 11 hours, 2 minutes ago
COVID-19 News: Yet again, but this time by researchers from UK, Pakistan and Qatar, are reporting clinical cases of patients with COVID-19 manifesting pneumomediastinum or mediastinal emphysema that can contribute to respiratory failure.
Pneumomediastinum, also known as mediastinal emphysema, is a condition in which air is present in the mediastinum (the space in the chest between the two lungs). This can be caused by a traumatic injury or in association with pneumothorax or other diseases.
Already previous reports were also acknowledged in a variety of peer reviewed journals reporting pneumomediastinum in COVID-19 patients though none to date have been covered in any
COVID-19 News coverages.
https://eurjmedres.biomedcentral.com/articles/10.1186/s40001-021-00585-9
https://www.cureus.com/articles/45075-air-should-not-be-there-a-case-of-pneumomediastinum-and-pneumopericardium-in-covid-19
https://www.mdpi.com/2543-6031/88/5/466
https://www.sciencedirect.com/science/article/pii/S1930043321005665
https://www.mdpi.com/2077-0383/10/23/5608
https://www.sciencedirect.com/science/article/pii/S2052297520301372
https://www.panafrican-med-journal.com/content/article/39/26/full/
The study team reported here two cases of COVID-19 patients aged 29 and 68 years who were diagnosed with pneumomediastinum (PM).
Though pneumomediastinum (PM) was initially a rare complication in COVId-19 patients, recently the rate on incidences of such occurrences seems to be increasing.
Patients with COVID-19 can present with a variety of etiologies that make them vulnerable to pneumomediastinum (PM).
Respiratory complications due to COVID-19 are widely known, and it presents as mild to severe and critical illness. Spontaneous pneumomediastinum (PM) is a known complication of COVID-19. Despite seeming to be a lesser-known condition, PM can have a significant impact on disease progression and prognosis.
The study team presented here two contrasting cases of pneumomediastinum (PM).
Case A
The first case involved a young male aged 29 years who arrived at the emergency department with the chief complaints of worsening shortness of breath for the past 5 days. On initial assessment, he was a lean young
man who could sit on his own. However, he was breathless and unable to speak in complete sentences. His general physical examination was remarkable for oxygen saturation of 84% on room air, heart rate of 110 beats per minute, and a raised respiratory rate of 30/minute. His recorded body temperature was in the normal range. His respiratory examination revealed bilateral crepitation, although the trachea was central and the percussion notes were dull. The rest of the systemic review was unremarkable.
The male patient had no background of any comorbidities or chronic illnesses. He was an active young gentleman who was otherwise fit and well. His family history of interest included VTE (Venous Thromboembolism) in a first-degree relative. The patient stated that he was single, lived alone, and managed his daily routine by himself. He denied any history of cigarette smoking but drank alcohol occasionally. There was no positive history of illicit drug use. Furthermore, there was no recent travel history, and he was not vaccinated against COVID-19.
He tested positive for COVID-19 on the reverse transcriptase-polymerase chain reaction (RT-PCR). His initial chest X-ray (CXR) revealed coalescing patchy consolidations in the peripheral and mid-to-lower zones, which were consistent with the symptoms of mild COVID. His initial levels were as follows: D-dimers, 1392 ng/mL; lactate dehydrogenase (LDH), 865 U/L; C-reactive protein (CRP), 39 mg/dL. Other laboratory results were remarkable for a white cell count of 3.4, a neutrophil count of 2.68, and a lymphocyte count of 0.64. His urea and electrolytes panel were unremarkable, except for the low levels of sodium (126 mmol/L). The initial venous blood gas obtained on admission revealed a pH of 7.421, PO2 of 6.40 kPa, PCO2 of 5.03 kPa, and bicarbonate level of 24.3 mmol/L.
As result of his condition, the patient was admitted to the acute medical unit and initiated on intravenous coamoxiclav, oral clarithromycin, and dexamethasone, in addition to 4 L of oxygen through a nasal cannula. During his stay, he was advised to be self-prone daily. With the aforementioned management plan in place, the patient was found to be settled and feeling better, which was ascertained by his improving respiratory and heart rates.
However, his oxygen requirement increased gradually, and he became more tachycardiac and tachypneic on the second day of admission (DOA). At this point, reassessment by the ward team led to a repetition of the measurement of his D-dimers to rule out PE (pulmonary embolism). Moreover, he was administered a high percentage of oxygen through a mask (40%).
Consequently, his D-dimer was found to be higher (4000 ng/dL) than that at the time of this admission (1392 ng/dL). In addition to the other clinical features, this observation raised suspicion about PE. Therefore, a treatment dose of low-molecular-weight heparin for PE was administered, and a computed topography-pulmonary angiogram (CTPA) was performed on the third DOA, albeit no embolus was identified in his pulmonary arteries. Nevertheless, the presence of air density in the mediastinum along with bilateral subcutaneous emphysema was noted in addition to peripheral ground-glass consolidation.
These clinical findings were consistent with pneumomediastinum or PM on the background of COVID-19 pneumonitis. Chest CT was performed, which consolidated the diagnosis of PM along with COVID-19 and esophageal pathology as the cause for the presence of air in the mediastinum.
It was found that on the sixth DOA, the patient started to show improvement. His oxygen saturation was maintained at 98–99% on 28% oxygen, and his other vitals were in the normal range. On the seventh DOA, his supplemental oxygen requirement improved, and his saturation was maintained at 97% on 2–3 L of oxygen. Accordingly, the study team decided to keep the patient under observation for another 24 h. On the eighth DOA, he was found to be feeling well and not requiring further oxygen supplementation, and he was discharged on oral antibiotics.
Case B
The second case study involve a male patient aged 68 years who presented with shortness of breath, dry cough, and mild chest discomfort on the ninth day after his positive COVID-19 PCR report. He was in respiratory distress on initial examination, as he was tachypneic (respiratory rate of 30) and could not speak in complete sentences. Moreover, the oxygen saturation in the room air was 85%, while his heart rate was 82 bpm, blood pressure was 114/63, and body temperature was 37°C. His respiratory examination revealed bilateral crackles on both lung fields. He had a background of hypertension and hypercholesterolemia. He was an active middle-aged man with a clinical frailty score of 3. 14 He was a nonsmoker, had never taken any form of alcohol, and had not received vaccination against SARS-CoV-2.
He was found positive for COVID-19 on RT-PCR. His initial CXR revealed bilateral patchy airspace consolidation in the peripheral mid and lower zones, which was consistent with the findings of COVID-19 pneumonia. His initial levels of D-dimers and CRP were 266 ng/mL and 43 mg/dL, respectively. The other laboratory studies revealed a white cell count of 3.4, a neutrophil count of 2.73, and a lymphocyte count of 0.35. The urea and electrolytes panel were found to be in the normal range.
The physicians initiated the patient on oral dexamethasone, intravenous coamoxiclav, and oral clarithromycin, as per the existing protocol. They also started him on 4 L of oxygen through a nasal cannula. The patient’s oxygen demand was increased to 15 L on the third DOA. However, on the fourth DOA, he developed hypoxia on 15 L of oxygen.
Subsequently the patient was put on continuous positive airway pressure (CPAP), which slowed his breathing rate and brought his oxygen saturation to 94%. On the seventh DOA, he maintained his saturation at the lowest possible settings of the CPAP machine. Accordingly, it was decided to wean him off CPAP to 15 L of oxygen through a nonrebreather mask.
However, at this time, the patient complained of chest pain, for which he was subjected to an ECG, a complete set of blood tests, and a CXR. His blood tests revealed a rising D-dimmer level (5221 ng/mL).
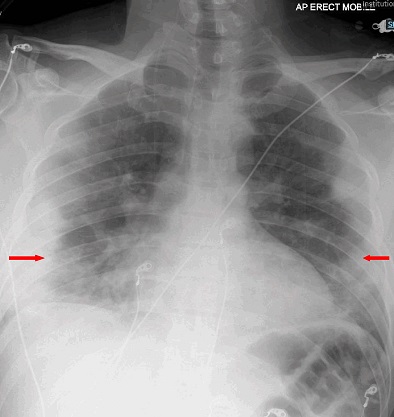
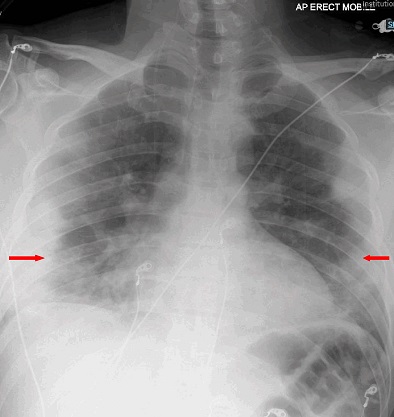
The cardiac cause of his chest pain was excluded based on the normal troponin levels and normal sinus rhythm on ECG. The radiologists reported his CXR as “air lucency along the lateral wall of the upper trachea, which represents a subtle PM.”
The patient’s chest pain worsened relative to his presenting symptoms, which were now associated with facial and periorbital swelling. His examination revealed neck and chest wall crepitus. Repeat CXR affirmed the diagnosis of subcutaneous emphysema in the neck and bilateral chest walls in addition to PM and patchy consolidation due to COVID-19, which were all found to be advancing.
These events coincided with his worsening hypoxia and severe dysphagia secondary to PM and progressive ARDS. Urgent thorax CT exhibited extensive surgical emphysema throughout the soft tissues of the thorax and lower neck. It also showed peripheral ground-glass changes throughout both lungs with patchy consolidations. The extensive PM was worse than that on the previous CXR, accordingly, CTPA was ruled out. As a result, the lung multidisciplinary team care decided to amend his escalation plan to ward-based care. The team believed that CPAP, NIV, and mechanical ventilation were not appropriate interventions to alleviate his ailments. It was agreed to manage his PM and subcutaneous emphysema conservatively. His oxygen saturation was persistently below the target, and his consciousness level was reduced. Eventually, after spending 22 days in the hospital, he passed away peacefully.
The case reports were published in the Qatar Medical Journal called Q Science.
https://www.qscience.com/content/journals/10.5339/qmj.2023.4
The study team concluded, “PM is a rare complication of COVID-19 pneumonia with significant lung involvement, which may or may not require invasive ventilatory support. However, the coexistence of PM with a significant parenchymal lesion on CT suggests serious alveolar membrane degradation and, consequently, a probable deterioration of the clinical outcomes. On the other hand, when the lung lesions are not severe, the clinical course appears to be better with an improved prognosis. Future research should include more numbers of patients to establish a correlation between PM and a potential prognostic factor.”
Thailand Medical News would like to add that currently lots of physicians are also reporting the occurrence of Pneumomediastinum (PM) in patients with COVID-19 associated pneumonia in China, Japan and also Italy where it is suspected the various BF sub-lineages including the BF.7.14 in China and new BF.5 variant with the ORF1A I2873V mutations in Japan could possibly be behind the rise of such infections.
https://www.thailandmedical.news/news/covid-19-news-deadly-covid-19-associated-pneumonia-rising-in-many-parts-of-the-world-including-italy,-china,-japan,-etc-are-the-bf-variants-at-play
https://www.thailandmedical.news/news/breaking-covid-19-news-is-the-new-bf-5-variant-with-orf1a-i2873v-mutation-driving-covid-19-deaths-in-japan-urgent-research-warranted
For the latest
COVID-19 News, keep on logging to Thailand Medical News.