Neutrophils Hijacked in COVID-19 and Lung Fibrosis Share Dangerous Inflammatory Pathways
Nikhil Prasad Fact checked by:Thailand Medical News Team Jun 12, 2025 8 months, 1 week, 4 days, 23 hours, 28 minutes ago
Thailand Medical News: Scientists Discover Striking Similarities in Immune Cell Behavior Between COVID-19 and Lung Fibrosis
In a major new discovery, researchers from multiple institutions across Greece have revealed that neutrophils—white blood cells crucial to fighting infections—are showing eerily similar and dangerous behavior in both COVID-19 and idiopathic pulmonary fibrosis (IPF), a chronic, non-infectious lung disease. This surprising overlap offers new clues into why both conditions can lead to severe, often irreversible damage to lung tissue.
 Neutrophils Hijacked in COVID-19 and Lung Fibrosis Share Dangerous Inflammatory Pathways
Neutrophils Hijacked in COVID-19 and Lung Fibrosis Share Dangerous Inflammatory Pathways
Neutrophils are usually first responders to infection, rushing in to fight invaders like viruses. But when they overreact or become chronically activated, they can cause more harm than good, triggering inflammation and damaging the very tissues they are supposed to protect. This
Thailand Medical News report uncovers how COVID-19 and IPF both hijack neutrophils and push them into a hyperinflammatory state that promotes severe lung injury and scarring.
The international research team included scientists from the Biomedical Research Foundation Academy of Athens (BRFAA), ‘Attikon’ General University Hospital, the University of Patras, Democritus University of Thrace, and ‘Sotiria’ General Hospital of Chest Diseases. They studied the gene activity of neutrophils isolated from COVID-19 and IPF patients, comparing them with those from healthy individuals.
What the Scientists Found Inside Neutrophils
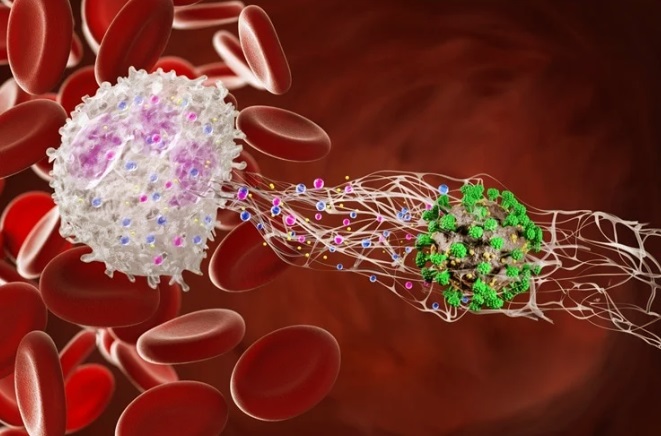
Using advanced RNA sequencing techniques, the team identified thousands of genes that were behaving abnormally in neutrophils from both COVID-19 and IPF patients. In both diseases, these immune cells were primed for what scientists call “NETosis”—a process where neutrophils release webs of DNA and enzymes, known as neutrophil extracellular traps (NETs), to trap and kill pathogens.
While NETs are helpful in fighting infections, their overproduction has been tied to tissue damage, blood clots, and chronic inflammation. The study found that in both COVID-19 and IPF patients, neutrophils had turned into NET-producing machines. Key pathways related to inflammation, immune signaling, chromatin remodeling (which prepares DNA for NET release), and even autophagy (a form of cellular cleanup) were hyperactive. At the same time, pathways related to protein production and metabolism were turned down, indicating that the cells were focusing all their energy on inflammatory responses rather than normal maintenance functions.
COVID-19 and IPF Share More Than Just Symptoms
When the researchers compared the neutrophil profiles of COVID-19 and IPF patients, they found that about 80% of the same genes were affected in both conditions. This overlap was startling and suggests that similar molecular pathways are at play, despite the different causes of these diseases—one being viral and the other not. The findings a
lso support earlier observations that some people who recover from COVID-19 later develop lung fibrosis.
To validate their findings, the researchers also examined lung tissue from IPF patients and observed clear signs of NET formation. Areas of the lung showed markers of histone H3 and myeloperoxidase—two key components of NETs—trapped within webs of DNA.
A New Role for Activin and Follistatin in Neutrophil Dysfunction
Another striking finding involved the Activin/Follistatin system, a set of molecules that regulate immune and growth-related functions in the body. This system was previously found to be disrupted in COVID-19 patients, and the new study now shows that this disruption correlates with changes in neutrophil behavior.
Higher levels of Activin-A, Activin-B, and Follistatin in the blood were linked to gene changes in neutrophils that drive inflammation and NET formation.
Interestingly, traditional blood markers like neutrophil count or the neutrophil-to-lymphocyte ratio did not show this correlation, suggesting that Activin and Follistatin may be more accurate markers of disease severity.
Why This Research Matters
The findings have big implications. First, they suggest that targeting neutrophils—and particularly their tendency to form NETs—could help treat both COVID-19 and IPF. Second, monitoring Activin and Follistatin levels in patients could help predict which cases might become severe. Lastly, these insights could lead to new therapies aimed at calming the immune system before it causes irreversible lung damage.
Drugs that block NET formation, such as DNase I (already used in cystic fibrosis), or those that target the TGF-β and Activin/Follistatin pathways, might offer new hope for patients struggling with lung inflammation due to either infection or chronic disease.
The Conclusion
This breakthrough research confirms that neutrophils play a central role in the progression of both COVID-19 and idiopathic pulmonary fibrosis. By mapping how these immune cells behave at a molecular level, the study has uncovered a shared inflammatory program that includes heightened NET formation, overactive immune signaling, and suppression of normal cellular maintenance. These discoveries open the door to new blood-based diagnostic tools and treatment strategies aimed at controlling neutrophil-driven damage in the lungs. Importantly, the data also highlight the Activin/Follistatin system as a potential biomarker and therapeutic target, offering a new lens through which to understand and manage respiratory diseases.
The study findings were published in the peer reviewed journal: Respiratory Research
https://link.springer.com/article/10.1186/s12931-025-03180-2
For the latest COVID-19 News, keep on logging to
Thailand Medical News.
Read Also:
https://www.thailandmedical.news/news/neutrophil-trap-genes-could-be-the-missing-link-between-long-covid-and-guillain-barre-syndrome
https://www.thailandmedical.news/news/beta-glucans-found-in-mushrooms-can-reprogram-neutrophils-to-combat-influenza-a-viruses
https://www.thailandmedical.news/news/neutrophil-elastase-inhibitor-sivelestat-for-covid-19-induced-ards
https://www.thailandmedical.news/articles/coronavirus
https://www.thailandmedical.news/pages/thailand_doctors_listings