Imperial College London Study Dispels Previous Findings That Immune Abnormalities Are Associated With Long COVID!
Thailand Medical News Team Aug 24, 2023 2 years, 5 months, 2 weeks, 6 days, 22 hours, 28 minutes ago
Long COVID: The world has been grappling with the ongoing challenges posed by Long COVID, a condition where individuals continue to experience symptoms long after their initial SARS-CoV-2 infection. Unraveling the mystery behind the persistence of these symptoms has been a priority for researchers, particularly when it comes to understanding how the immune response plays a role. Imperial College London has taken a significant step forward by conducting a study that sheds light on this complex issue.
 The Enigma of Long COVID and Immunity
The Enigma of Long COVID and Immunity
Long COVID refers to the continuation of symptoms for more than four weeks after the initial infection with the SARS-CoV-2 virus. Some studies suggest that around 20% of individuals are affected by this condition, with symptoms lingering even two years after the initial infection. These symptoms encompass a wide range of issues, including fatigue, pain, breathing difficulties, cardiovascular problems, neurological challenges, and cognitive impairments.
Despite the growing recognition of
Long COVID, there's a lack of clarity due to factors like the absence of standardized diagnostic tests and clinical criteria. One hypothesis is that abnormalities in the immune response during the acute infection phase could contribute to the persistence of symptoms. This raises the question of whether people with Long COVID have either weak or overly strong immune responses during the initial infection.
Imperial College London's Groundbreaking Study
To address this critical question, researchers at Imperial College London conducted a meticulous study involving 86 healthcare workers who had experienced mild or asymptomatic SARS-CoV-2 infections during the first wave of the pandemic. These individuals were divided into two groups: those who developed persistent symptoms and those who didn't. By closely analyzing their immune responses, the researchers aimed to determine if there were any significant differences that could explain the persistence of symptoms.
The study involved evaluating both the humoral (antibody-based) and cellular (T cell-based) immune responses to the SARS-CoV-2 virus. Researchers also examined the levels of antibodies against specific viral components, the virus-neutralizing capacity of the immune response, and the behavior of T cells. This comprehensive approach allowed them to gain insights into the immune mechanisms at play.
Surprising Findings Dispel Immune Abnormality Hypotheses
The results of the study were surprising yet illuminating. The study team found that there were no meaningful differences in the immune responses between those who experienced persistent symptoms and those who didn't. This observation held true both in the early stages, up to 18 weeks post-infection, and even after a year and two vaccine doses.
These findings are significant as they challenge the prevailing hypotheses that Long COVID is linked to quantitative differences in the immune response during the acute infection phase. In simpler terms, the study suggests that the strength of the immune response doesn't seem to be the main driver behind the persistence of symptoms. This finding contradict
s the notion that individuals with Long COVID either have weaker immune responses or excessive immune reactions.
An In-Depth Look at the Study
The study was conducted with a rigorous approach. The researchers collected data from healthcare workers, a group that provides a unique perspective due to their regular exposure to the virus. This allowed for the monitoring of immune responses over time, both before and after vaccination. Importantly, the study design accounted for factors like symptom reporting bias and used a controlled group for comparison.
By focusing on both the antibody and T cell responses, the researchers covered two key aspects of the immune system's defense against the virus. Antibodies are proteins that specifically target viral components, while T cells play a crucial role in orchestrating immune responses. By analyzing these two aspects, the researchers gained a comprehensive understanding of the immune landscape.
During the period up to 18-weeks post-infection, the study team observed no difference in antibody responses to spike RBD or nucleoprotein, virus neutralization, or T cell responses. Also, there is no difference in the profile of antibody waning. Analysis at 1-year, after two vaccine doses, comparing those with persistent symptoms to those without, again shows similar SARS-CoV-2 immunity. Thus, quantitative differences in these measured parameters of SARS-CoV-2 adaptive immunity following mild or asymptomatic acute infection are unlikely to have contributed to Long Covid causality.
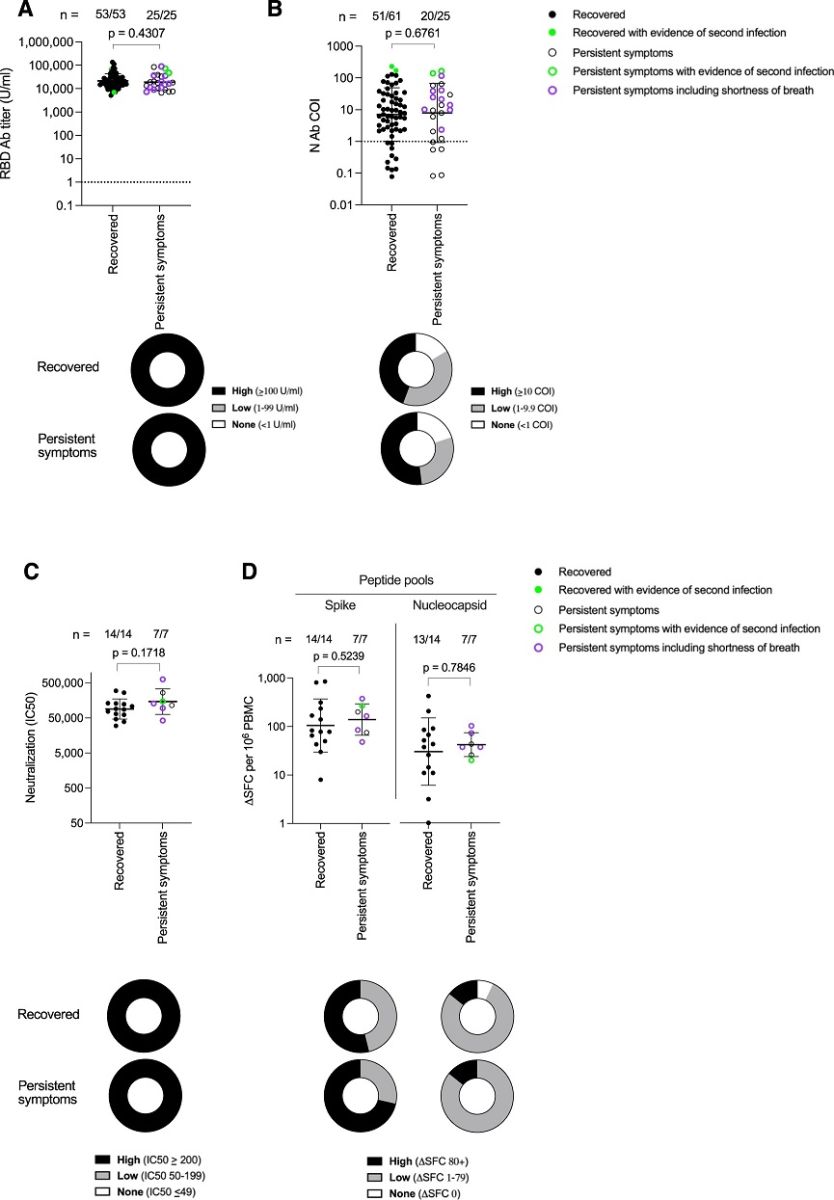 Antibody and T cell responses against SARS-CoV-2 at 12 months after laboratory confirmed infection in HCW that either Recovered or reported Persistent symptoms.
Antibody and T cell responses against SARS-CoV-2 at 12 months after laboratory confirmed infection in HCW that either Recovered or reported Persistent symptoms.
A S1 RBD (Recovered, closed circle, n = 53, 40% male); Persistent symptoms, open circle, n = 25, 28% male) and B Nucleocapsid antibody (Recovered, closed circle, n = 61, 34% male; Persistent symptoms, open circle, n = 25, 28% male) titers in HCW 12 months after laboratory confirmed SARS-CoV-2 infection. S1 RBD data is plotted for HCW who had received 2 doses of COVID-19 vaccine at the time of the 12-month blood sample. Numbers of HCW with a positive antibody titer are shown at the top of each plot. The proportion of HCW with a high (black), low (grey) or no antibody (white) titer is shown in doughnut plots below. Fifteen Recovered HCW (closed circle, 57% male) and 7 HCW with Persistent symptoms (open circle, 57% male) were assayed for C Neutralizing antibody IC50 against live ancestral (Wuhan Hu-1) SARS-CoV-2 virus and D T cell responses against spike and nucleocapsid mapped epitope peptide pools, 12 months after laboratory confirmed SARS-CoV-2 infection. Numbers of HCW showing a positive neutralizing antibody or T cell response for each assay are shown at the top of each plot. The proportion of HCW in each group with a high (black), low (grey) or no response (white) (as defined in each key) are represented by doughnut plots below. Two-tailed Mann-Whitney U test (Graphpad Prism version 8.0) was used to test for significant differences between Recovered HCW and those reporting Persistent symptoms. Source data are provided as a Source Data file. HCW with serological evidence of a subsequent SARS-CoV-2 re-infection between 6 and 12 months are annotated in green. HCW who reported persistent shortness of breath at 12 months are shown as purple open circles. Error bars shown are geometric mean + 1 geometric SD. Ab antibody, COI cut-off index, HCW health care workers, N nucleocapsid, PBMC peripheral blood mononuclear cells, RBD receptor binding domain, SD standard deviation, SFC spot forming cells, U units.
Implications and Future Research
This study from Imperial College London has several important implications. First, it suggests that Long COVID isn't primarily driven by differences in the immune responses to the virus. This challenges the prevailing theories that either weak or hyperactive immune responses are responsible for the condition's persistence.
While this study sheds light on certain aspects of Long COVID, it's important to note that the condition is still not fully understood. The complexity of its underlying mechanisms is likely multifaceted, involving interactions between the virus, the immune system, and other physiological factors.
Future research will continue to unravel the mysteries of Long COVID, exploring additional factors that could contribute to the condition's persistence. These might include viral reservoirs in the body, immune memory, and the potential role of other infections. By piecing together these intricate puzzle pieces, scientists aim to develop more effective strategies for the prevention and management of Long COVID.
In conclusion, Imperial College London's study has provided valuable insights into the relationship between immune responses and Long COVID. The findings challenge existing theories and pave the way for further research to decipher the complex nature of this condition. As the world continues to grapple with the aftermath of the pandemic, understanding and addressing Long COVID remains a crucial scientific endeavor.
The study findings were published in the peer reviewed journal: Nature Communications.
https://www.nature.com/articles/s41467-023-40460-1
For the latest on
Long COVID, keep on logging to Thailand Medical News.
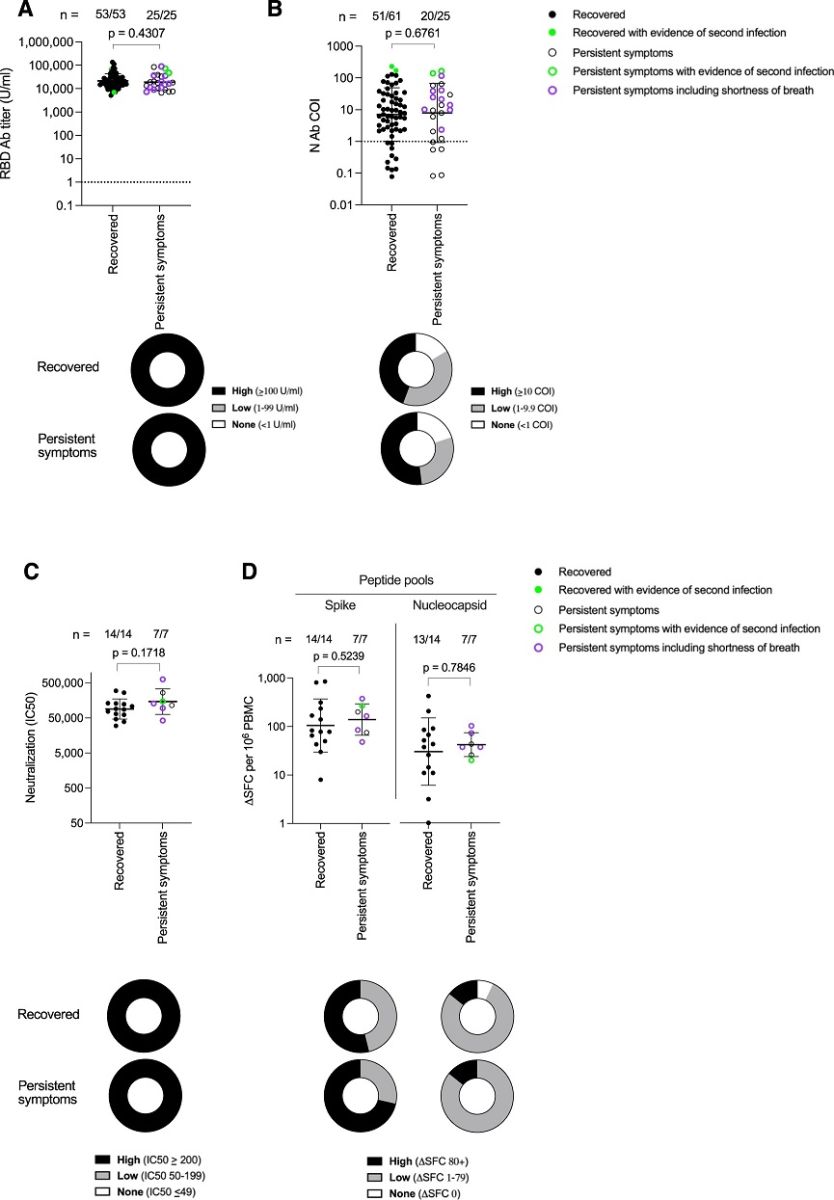 Antibody and T cell responses against SARS-CoV-2 at 12 months after laboratory confirmed infection in HCW that either Recovered or reported Persistent symptoms.
Antibody and T cell responses against SARS-CoV-2 at 12 months after laboratory confirmed infection in HCW that either Recovered or reported Persistent symptoms.