Nikhil Prasad Fact checked by:Thailand Medical News Team May 30, 2025 8 months, 3 weeks, 4 days, 29 minutes ago
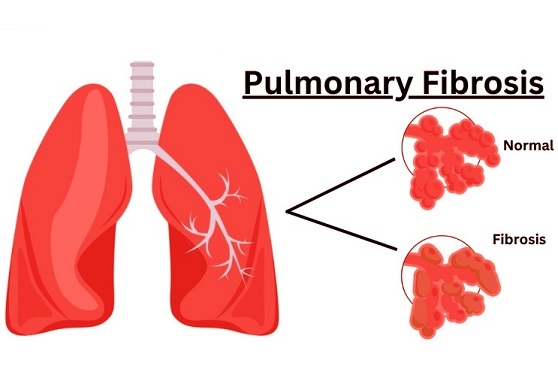
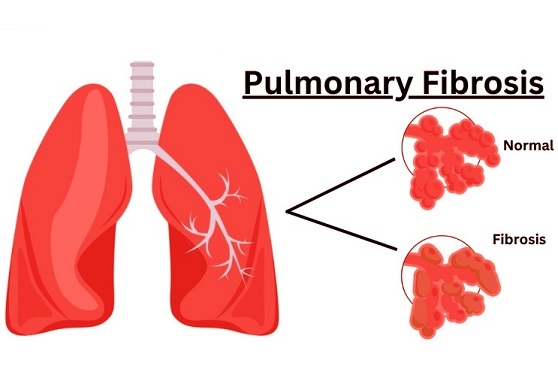
Medical News: A new study by researchers from the University of Groningen’s University Medical Center Groningen in the Netherlands is drawing attention to a dangerous and long-lasting health issue linked to COVID-19—persistent lung scarring or fibrosis. This worrying consequence of the virus, known as post-COVID pulmonary fibrosis (PCPF), could affect millions of people worldwide, even years after they recover from the initial infection.
 Hidden Lung Damage in Millions Post COVID May Be Permanent and Irreversible
Hidden Lung Damage in Millions Post COVID May Be Permanent and Irreversible
According to the research team—Emma C.A. Vreeman, Janesh Pillay, and Janette K. Burgess—post-acute sequelae of COVID-19 (PASC), commonly referred to as long COVID, affects around 10 percent of COVID survivors. Many of these individuals report ongoing respiratory problems. This
Medical News report uncovers how some of these issues are tied to fibrotic lesions or scars in the lungs that don’t seem to go away and could even worsen over time.
Lung Damage Can Persist for Years
The study found that up to 45 percent of hospitalized COVID-19 patients developed signs of fibrotic lung damage just months after being discharged. These signs included shortness of breath, reduced lung capacity, and abnormalities visible in CT scans, such as ground-glass opacities and tissue scarring.
Worryingly, the researchers compared the long-term effects of COVID-19 to those observed in survivors of the original SARS outbreak in 2003. In that epidemic, some patients still showed lung damage 15 years later. The new data suggest that SARS-CoV-2 could trigger a similar permanent condition in a significant percentage of people.
Why Does This Happen
Scientists believe that the body’s attempt to repair lung tissue after severe COVID-19 can go awry. This process involves inflammation and activation of fibroblasts—cells responsible for tissue healing. However, when this repair process becomes excessive or disordered, it leads to the overproduction of collagen and other structural proteins that form scar tissue, making the lungs stiff and less effective at delivering oxygen.
Moreover, the virus may interfere with a protective lung enzyme known as ACE2. Normally, ACE2 helps regulate inflammation and tissue repair. But SARS-CoV-2 hijacks this enzyme to enter cells. As a result, the protective effects of ACE2 are reduced, and harmful substances like angiotensin II build up, further fueling lung fibrosis.
New and Emerging Treatments
Currently, two drugs—pirfenidone and nintedanib—are used to slow down lung fibrosis. But these medications only limit the progression of the disease; they do not reverse it. Promising alternatives include histone deacetylase inhibitors (HDACi), angiotensin receptor blockers (ARBs), and even experimental cell therapies using mesenchymal stem cells (MSCs) or lung spheroid cells. These therapies aim not just to halt, but potentially to reverse fibrotic changes in the lungs.
Biomarkers
such as elevated collagen breakdown products and integrin subunits are also being explored to detect early signs of lung damage and intervene sooner.
What This Means for the Future
The researchers warn that although PCPF is not expected to worsen progressively over time, it can still persist indefinitely in some individuals, affecting their breathing, quality of life, and overall health. Even a small percentage of people developing this condition after infection translates to millions globally—especially given the sheer scale of COVID-19’s spread.
Healthcare systems must prepare for this long-term consequence by investing in diagnostics, rehabilitation, and research into effective treatments.
In conclusion, persistent lung scarring following COVID-19 presents a silent but significant threat to global health. A small yet substantial portion of survivors may live with permanent respiratory limitations, despite having seemingly recovered from the acute phase. Identifying and treating these cases early with targeted therapies—especially those capable of reversing fibrotic damage—will be vital. For now, early treatment and monitoring remain the best tools for reducing long-term complications.
The study findings were published in the peer reviewed journal: Pharmacology and Therapeutics
https://www.sciencedirect.com/science/article/pii/S0163725825001032
For the latest COVID-19 News, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/ccl2-ccr2-axis-and-its-role-in-pulmonary-fibrosis-from-respiratory-viruses
https://www.thailandmedical.news/news/favipiravir-that-was-used-to-treat-covid-19-actually-causes-lung-inflammation-lung-damage-and-lung-fibrosis
https://www.thailandmedical.news/news/covid-19-causes-inflammation-tissue-injury-and-fibrosis-of-the-respiratory-tract-and-lungs
https://www.thailandmedical.news/articles/coronavirus
https://www.thailandmedical.news/pages/thailand_doctors_listings