Neutrophil Trap Genes Could Be the Missing Link Between Long COVID and Guillain Barre Syndrome
Nikhil Prasad Fact checked by:Thailand Medical News Team May 15, 2025 8 months, 4 weeks, 1 day, 23 hours, 38 minutes ago
Medical News:
Chinese Scientists Discover Overlapping Molecular Clues Behind Nerve Damage Seen in Post COVID Syndrome
In a groundbreaking study conducted by researchers from the Department of Neurology at The Eighth Affiliated Hospital and Sun Yat-sen Memorial Hospital, both under Sun Yat-sen University in China, scientists have identified a possible molecular link between COVID-19 and Guillain-Barre Syndrome (GBS), a rare but serious neurological disorder. The study focuses on the role of neutrophil extracellular traps (NETs)—a component of the immune system—as a potential trigger behind nerve damage in patients who develop GBS after recovering from COVID-19.
 Neutrophil Trap Genes Could Be the Missing Link Between Long COVID and Guillain Barre Syndrome
Neutrophil Trap Genes Could Be the Missing Link Between Long COVID and Guillain Barre Syndrome
This
Medical News report covers the work of researchers: Hua Su, Dan-Yu Lin, Xiao-Huan Liu, Jie-Li Zhang, Zhong-Gui Li, En-Xiang Tao, and Kai-Xun Huang, who used advanced bioinformatics tools to analyze gene expression data from blood samples of both COVID-19 and GBS patients. Their aim was to uncover common patterns and mechanisms that might explain why some people develop GBS as a delayed immune response following SARS-CoV-2 infection.
Shared Immune Pathways and Inflammatory Triggers Uncovered
Using data from six Gene Expression Omnibus (GEO) datasets, the researchers pinpointed 145 genes that were expressed abnormally in both COVID-19 and GBS patients. These genes were mainly involved in immune system regulation and inflammation, supporting the theory that GBS in post-COVID patients may not be caused directly by the virus itself but rather by a delayed autoimmune reaction.
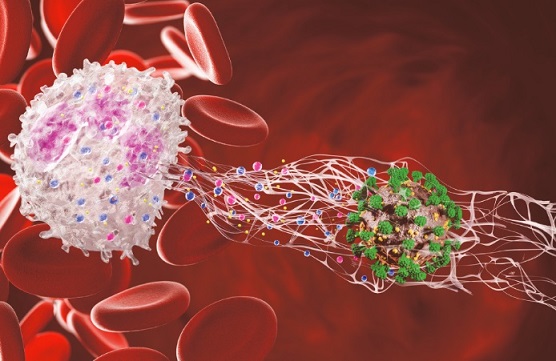
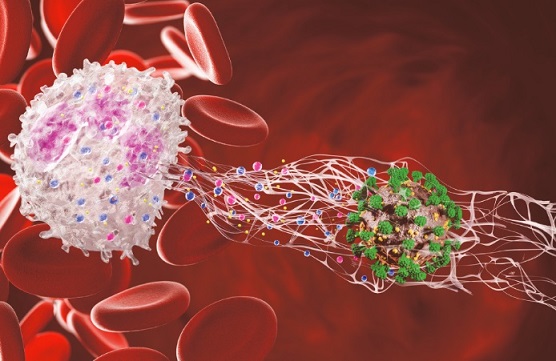
Three genes in particular—MMP9, CAMP, and CASP1—stood out as key culprits. These genes are involved in the formation of neutrophil extracellular traps or NETs, which are web-like structures released by white blood cells to trap pathogens. However, when overproduced, NETs can lead to excessive inflammation and tissue damage, potentially contributing to autoimmune conditions like GBS.
Functional analysis revealed that these three NET-related genes were highly active in both diseases, especially in patients with more severe symptoms. MMP9, which breaks down extracellular matrix components, was shown to promote tissue damage and inflammatory processes. CASP1 plays a central role in activating inflammatory proteins and is linked to a process known as pyroptosis, a form of programmed cell death that further amplifies immune responses. CAMP, on the other hand, encodes a protein called LL-37 which can enhance immune signaling but may also contribute to hyperinflammation when unregulated.
Neutrophils and Macrophages Identified as Key Players
Further analysis revealed that neutrophils and macrophages—the body’s frontline immune cells—were significantly more active in the blood of both COVID-19 and GBS patients. These cells are known to interact closely during immune responses and are responsible for triggerin
g NETs production. Their excessive presence and activity could explain the sustained inflammation observed in post-COVID GBS cases.
Interestingly, a reduction in beneficial immune cells such as CD8 T cells and natural killer cells was also observed. This imbalance between immune activation and regulation may create a harmful environment that damages peripheral nerves, leading to GBS symptoms such as muscle weakness, tingling, and even paralysis.
Potential Drug Candidates Offer New Hope
The team also used a computational method to screen for drugs that could counteract the harmful effects of the identified genes. They found ten promising compounds, including BI-2536 and TG-101348, which target inflammatory pathways and could be repurposed to treat post-COVID GBS. These drugs were identified using the Connectivity Map (cMap) database, which compares gene expression profiles of diseases with those modified by known drug compounds.
Conclusions and Outlook
The findings of this study highlight a potentially critical mechanism behind the development of Guillain-Barre Syndrome following COVID-19. By identifying MMP9, CASP1, and CAMP as core NETs-related genes shared between both diseases, the study provides compelling evidence that excessive immune responses—particularly those involving neutrophils and macrophages—play a central role in nerve damage. The consistent upregulation of these genes and their association with inflammatory markers suggest that targeting NET formation and its associated pathways may offer new therapeutic strategies for patients suffering from post-COVID-19 GBS. Importantly, the study paves the way for future research that could validate these findings in clinical settings and develop targeted treatments to prevent long-term neurological complications after COVID-19.
The study findings were published in the peer reviewed journal: Frontiers in Neurology.
https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2025.1447725/full
For the latest on Long COVID, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/university-of-connecticut-study-warns-that-long-covid-is-quietly-damaging-the-brain-and-mental-health-of-thousands
https://www.thailandmedical.news/news/low-dose-naltrexone-could-be-the-key-to-reversing-immune-dysfunction-in-long-covid-patients
https://www.thailandmedical.news/news/dietary-supplements-emerge-as-possible-relief-for-long-covid-pain-sufferers
https://www.thailandmedical.news/articles/long-covid
https://www.thailandmedical.news/pages/thailand_doctors_listings