Doctors Warn That COVID-19 Blood Thinning Treatment to Prevent Clots Can Trigger Internal Bleeding Shock
Nikhil Prasad Fact checked by:Thailand Medical News Team Jan 03, 2026 1 month, 3 weeks, 15 hours, 12 minutes ago
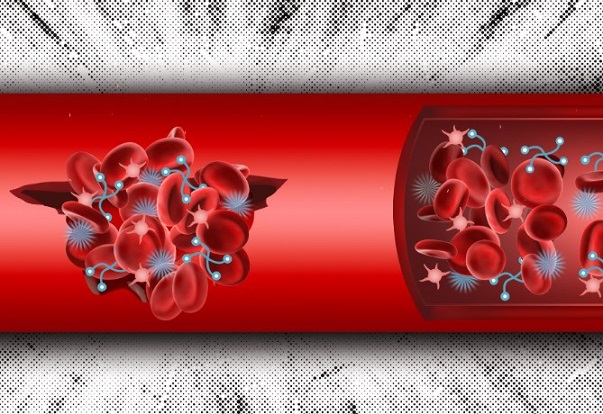
Medical News: Doctors in China have reported a rare and life-threatening complication in a patient being treated for severe COVID-19 infection. A 63-year-old woman developed sudden internal bleeding in her abdominal wall while receiving blood thinning medication meant to prevent dangerous clots. The case highlights how lifesaving treatments can sometimes carry serious risks especially in patients with complex underlying illnesses.
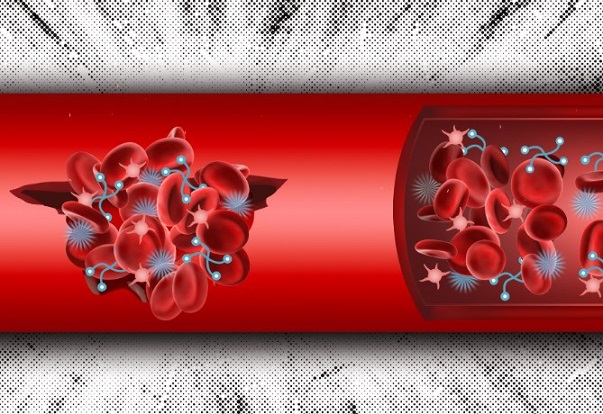 A COVID-19 patient on blood thinners suffers sudden internal bleeding revealing hidden dangers of standard treatments
A COVID-19 patient on blood thinners suffers sudden internal bleeding revealing hidden dangers of standard treatments
This
Medical News report draws attention to the need for careful and personalized care in high risk COVID patients.
The patient was admitted to Zibo Central Hospital which is affiliated with Binzhou Medical University in Shandong China. The research team also included specialists from Shanghai East Hospital and Tongji University in Shanghai. The woman had a known kidney condition called membranous nephropathy and was taking steroid medication long before she contracted COVID-19.
Why blood thinners were used
Severe COVID-19 is known to increase the risk of blood clots which can cause strokes lung blockages and organ failure. To prevent this, doctors often give anticoagulant drugs also called blood thinners. In this case the patient was given dalteparin a commonly used low dose anticoagulant while she was hospitalized and later while in intensive care.
Sudden collapse and emergency surgery
After showing signs of recovery and being removed from a breathing machine, the patient suddenly developed severe abdominal pain and low blood pressure. Her hemoglobin levels dropped sharply indicating massive blood loss. Scans revealed a large internal bleed caused by a ruptured inferior epigastric artery which is a blood vessel deep in the abdominal wall.
Doctors immediately stopped the blood thinner gave blood transfusions and performed emergency surgery to tie off the bleeding artery. The quick response saved her life.
Why this case is important
The study explains that COVID-19 itself can damage blood vessels and disturb normal clotting. At the same time kidney disease can cause blood thinners to build up in the body even when given at standard doses. Steroid treatment may further weaken blood vessels. Together these factors created a perfect storm leading to spontaneous bleeding without any injury.
Importantly the researchers ruled out injection related injury showing that the bleeding was not caused by how the drug was administered but by the body’s altered response.
Recovery and long-term outcome
The patient gradually recovered and was discharged after 46 days in hospital. Follow up at three months showed no further bleeding no blood clots and stable kidney function. Doctors decided not to restart anticoagulant therapy due to the severity of the earlier bleeding episode.
&a
mp;nbsp;
Conclusions
This case clearly shows that while blood thinners save lives in COVID-19, they can also cause rare but catastrophic bleeding especially in patients with kidney disease and those on steroids. The findings stress the importance of individualized treatment close monitoring and teamwork between intensive care kidney and blood specialists to balance clot prevention against bleeding risk.
The study findings were published in the peer reviewed journal: Frontiers in Medicine.
https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1728723/full
For the latest COVID-19 news, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/articles/coronavirus
https://www.thailandmedical.news/articles/long-covid