Nikhil Prasad Fact checked by:Thailand Medical News Team Feb 09, 2026 1 hour, 59 minutes ago
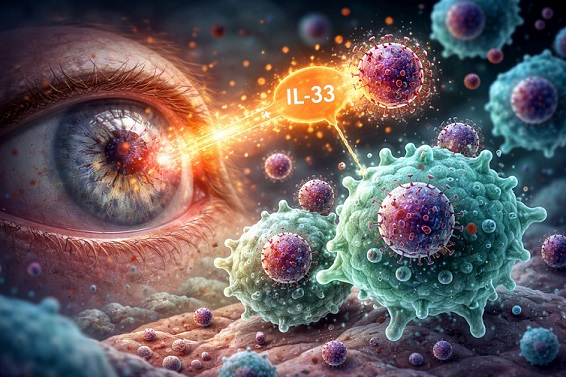
Medical News: Herpes simplex keratitis is one of the world’s leading infectious causes of vision loss, often striking without warning and recurring despite treatment. Now, new research suggests that a naturally occurring immune signal may reprogram the body’s own defense cells to better fight the virus before severe eye damage occurs.
 New research shows how reprogramming immune cell metabolism may help the eye fight herpes virus
New research shows how reprogramming immune cell metabolism may help the eye fight herpes virus
infections more effectively
A Closer Look at Immune Cells in the Eye
Herpes simplex keratitis is caused by herpes simplex virus type 1, which infects the cornea and can lead to pain, scarring, and even blindness. Current treatments rely heavily on antiviral drugs and steroids, but these approaches face problems such as drug resistance, side effects, and frequent relapses.
In this
Medical News report, researchers explored whether a signaling molecule called interleukin-33, or IL-33, could strengthen the eye’s immune response in a more targeted and durable way.
The study was conducted by scientists from the Department of Ophthalmology and the Department of Burns and Plastic Surgery at Nanjing Drum Tower Hospital, Medical School of Nanjing University, China, together with collaborators from The Eye Hospital of Wenzhou Medical University, China.
How IL-33 Reprograms Immune Defenders
The researchers focused on macrophages, immune cells that act as the body’s frontline virus fighters. Laboratory experiments showed that when macrophages were exposed to IL-33, they shifted into a special antiviral form known as CD169-positive macrophages. These cells were better at recognizing, trapping, and breaking down herpes virus particles.
IL-33 treatment also boosted markers linked to immune alertness and antigen presentation, meaning the macrophages could signal other immune cells more effectively. As a result, viral replication inside these cells dropped significantly.
Metabolism Turns Out to Be the Key
To understand why IL-33 made such a difference, the team analyzed both gene activity and metabolic changes inside the macrophages. They discovered that IL-33 rewired how these cells use fats and amino acids for energy.
A critical pathway involved an enzyme called lipoprotein lipase and a fat-derived molecule known as palmitoylcarnitine. Together, this metabolic axis gave macrophages the fuel needed to sustain strong antiviral activity. When this pathway was blocked, the protective effects of IL-33 largely disappeared.
Testing the Strategy in Living Eyes
The researchers then tested the approach in mice. Macrophages treated with IL-33 were transferred to the eye before herpes infection. These mice developed milder corneal damage, clearer corneas, and far lower viral levels compared to untreated animals. Blocking the metabolic pathway removed this benefit, while restoring key metabolites partially broug
ht protection back.
Why This Matters Going Forward
The conclusions from this work are significant. By showing that immune protection can be strengthened through metabolic reprogramming rather than direct antiviral drugs, the study opens the door to new preventive or supportive therapies. Such approaches could reduce reliance on steroids and limit long-term eye damage while working alongside existing treatments.
The study findings were published in the peer reviewed journal: Pharmaceuticals.
https://www.mdpi.com/1424-8247/19/2/285
For the latest on herpes research, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/articles/stds
https://www.thailandmedical.news/articles/ophthalmology-(eye-diseases)