BREAKING! Study Shows That COVID-19 Can Cause Intestinal Ischemia And Gastrointestinal Issues In Asymptomatic Individuals Who Continue To Test Negative!
Source: Medical News-SARS-CoV-2-Gastrointestinal Issues Nov 18, 2021 4 years, 3 months, 1 week, 1 hour, 22 minutes ago
Contrary to the fallacy that most idiots and ignorant experts claim that those who were COVID-19 asymptomatic have nothing to worry about, in reality the fact that the virus is able to disrupt the host immune systen such that no symptoms appear while the virus is still persistent in some deeper tissues or hard to reach organs for normal existing diagnostic platforms is actually worrisome.
Already many studies are emerging that many heart, kidney and neurological conditions can arise even in those that were COVID-19 asymptomatic, in what is being termed as long COVID or PASC (Post-acute Sequelae of COVID-19) and in some cases with fatal consequences. Then there are also studies and autopsies that have demonstrated viral persistence not only in those that were symptomatic but also in the asymptomatic.
In a new study by researchers from the University of Ferrara-Italy and the University Hospital of Ferrara Arcispedale Sant'Anna-Italy, it was found that bowel or intestinal ischemia and, in some cases, gastrointestinal issues were an onset of COVID-19 in otherwise asymptomatic patients with persistently negative swab.
The study findings were published in the peer reviewed Journal of Internal Medicine.
https://onlinelibrary.wiley.com/doi/10.1111/joim.13385
According to the study team, asymptomatic patients with Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) can develop hypercoagulable conditions and acute vascular events.
The main objective of the study was to determine whether SARS-CoV-2 was present in resected specimens from patients with acute bowel ischemia, but asymptomatic for Coronavirus Disease 2019 (COVID-19) and with persistently real-time polymerase chain reaction negative pharyngeal swab.
Three consecutive patients presented severe abdominal symptoms due to extensive ischemia and necrosis of the bowel, with co-existent thrombosis of abdominal blood vessels. None had the usual manifestations of COVID-19, and repeated pharyngeal swabs tested negative. They underwent emergency surgery with intestinal resection. Immunohistochemical testing for SARS-CoV-2 on resected tissue was performed.
Shockingly
, all tested samples were strongly positive for SARS-CoV-2.
This is the first case report in which patients with severe intestinal symptoms presented a marked SARS-CoV-2 positivity in the resected tissues, without any usual clinical manifestations of COVID-19.
These study findings suggest that the patients might be infected with SARS-CoV-2 presenting acute abdominal distress but without respiratory or constitutional symptoms.
As a confirmation of the possible involvement of the gastrointestinal tract in COVID-19 patients, past study data report nausea/vomiting symptoms in 5% and diarrhea in 3.8% of COVID-19 patients. However, SARS-CoV-2 presence was not previously reported in gastrointestinal samples.
https://www.nejm.org/doi/full/10.1056/nejmoa2002032
It seems unlikely that a virus that gains entry to the body via the respiratory tract and whose typical manifestations are mainly respiratory, should primarily infect the gut. However, in COVID-19 patients whose respiratory symptoms have sub-sided, the
virus may persist in the intestines for an extended period.
In a meta-analysis, viral RNA was found in the feces of 48% (95% CI, 38.3–57.9) of COVID-19 patients, even if the 70.3% (95% CI, 49.6–85.1) was SARS-CoV-2 negative in oro/nasopharyngeal samples.
https://pubmed.ncbi.nlm.nih.gov/32251668/
https://pubmed.ncbi.nlm.nih.gov/33033172/
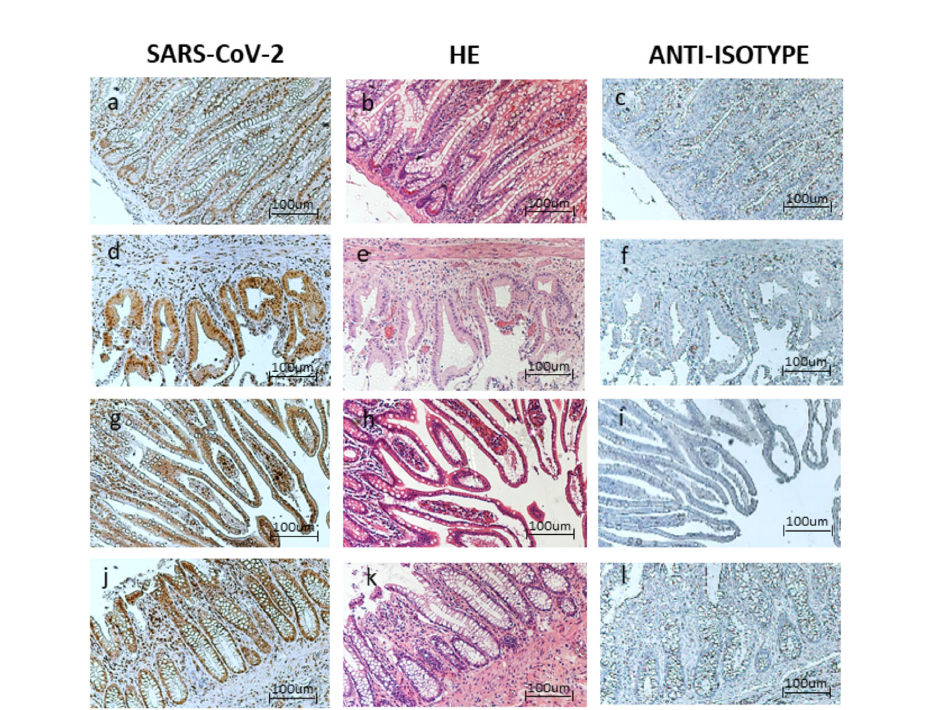 Case 1: Optical microscopy. Immunohistochemistry (IHC), 10x positive staining for (a) Acute Respiratory SyndromeCoronavirus 2 (SARS-CoV-2) virus, (b) hematoxylin-eosin, (c) anti-isotype staining. Case 1: Optical microscopy. IHC, 10xpositive staining for (d) SARS-CoV-2 virus, (e) hematoxylin-eosin, (f) anti-isotype staining. Case 2: Optical microscopy. IHC,10x positive staining for (g) SARS-CoV-2 virus, (h) hematoxylin-eosin, (i) anti-isotype staining. Case 3: Optical microscopy.IHC, 10x positive staining for (j) SARS-CoV-2 virus, (k) hematoxylin eosin, (l) anti-isotype staining
Case 1: Optical microscopy. Immunohistochemistry (IHC), 10x positive staining for (a) Acute Respiratory SyndromeCoronavirus 2 (SARS-CoV-2) virus, (b) hematoxylin-eosin, (c) anti-isotype staining. Case 1: Optical microscopy. IHC, 10xpositive staining for (d) SARS-CoV-2 virus, (e) hematoxylin-eosin, (f) anti-isotype staining. Case 2: Optical microscopy. IHC,10x positive staining for (g) SARS-CoV-2 virus, (h) hematoxylin-eosin, (i) anti-isotype staining. Case 3: Optical microscopy.IHC, 10x positive staining for (j) SARS-CoV-2 virus, (k) hematoxylin eosin, (l) anti-isotype staining
One can hypothesize that these three patients were infected with SARS-CoV-2, which remained asymptomatic at the respiratory level, but evolved in gastrointestinal pathogenesis. The negative results of the oro/nasopharyngeal samples might be due to the limit of detection of the test, especially in late infections.
https://www.frontiersin.org/articles/10.3389/fpubh.2020.593491/full
Importantly the presence of the virus in the gastrointestinal tissues suggests the transmission of the infection from the respiratory tract to the gastrointestinal compartment via intestinal blood vessels, perhaps in relation to declining levels of neutralizing antibodies, particularly Immunoglobulin A (IgA).
IgA is principally expressed in the body’s mucous membranes, particularly in the respiratory and gastrointestinal tracts where IgA is involved in the control of viral infections as the earliest neutralizing anti-body response to SARS-CoV-2 infection.
https://pubmed.ncbi.nlm.nih.gov/24348474/
https://pubmed.ncbi.nlm.nih.gov/33288662/
These three cases might be representative of an acute gastrointestinal infection/re-infection with SARS-CoV-2, that developed in severe gastrointestinal symptoms without affecting the respiratory tract.
The study data suggest the fecal-oral infection/re-infection as a possible alternative way of SARS-CoV-2 spreading, which deserves further investigation.
In fact, even more, evidence suggests that, like other related viruses, SARS-CoV-2 may also bean enteric virus that can infect via the fecal-oral route, possibly via angiotensin-converting enzyme2 expression in the gut.
https://pubmed.ncbi.nlm.nih.gov/32353371/
Such a hypothesis, together with the presence of SARS-CoV-2 RNA in the feces of COVID-19 patients, underlines the possible presence of potentially infectious materials, such as stools or baby diapers, that might increase the viral persistence in the environment.
https://pubmed.ncbi.nlm.nih.gov/32836117/
Corresponding author, Dr Angelina Passaro from the Department of Translational Medicine, University of Ferrara told Thailand
Medical News, “In conclusion, our study findings underline the importance to evaluate the possible presence of SARS-CoV-2 gut infection during the clinical practice, since patients without evident respiratory symptoms might develop severe abdominal events due to gut infection. We are aware of the limit of this research, due to the limited number of samples, that deserve further investigation. However, we hypothesize that the gastrointestinal tract can act as a virus reservoir even when the oro-nasal swab is negative. We suggest testing for SARS-CoV-2 presence in the resected samples of recent emergency cases of intestinal ischemia. This evaluation might increase the number of victims of the SARS-CoV-2 pandemic than currently suspected.”
Thailand Medical News would like to add, there is growing evidence that the new emerging Delta subvariants are evolving such their pathogenesis is moving more towards affecting the gastrointestinal tract as more patients being infected with these new sub-variants are displaying a new but wide array of gastrointestinal issues.
For the latest
SARS-CoV-2 News, keep on logging to Thailand Medical New
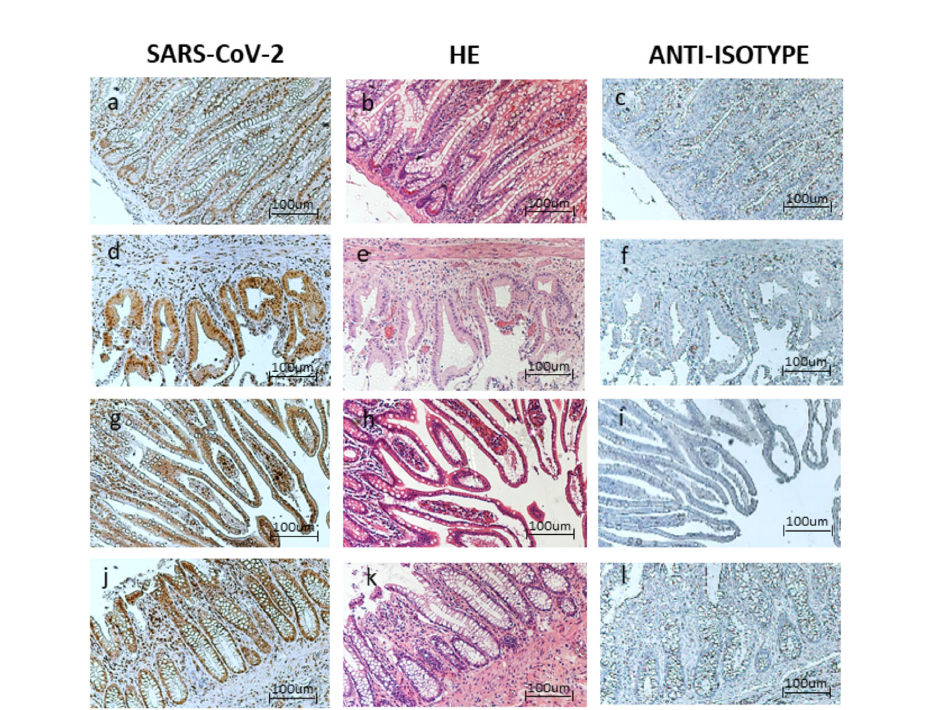 Case 1: Optical microscopy. Immunohistochemistry (IHC), 10x positive staining for (a) Acute Respiratory SyndromeCoronavirus 2 (SARS-CoV-2) virus, (b) hematoxylin-eosin, (c) anti-isotype staining. Case 1: Optical microscopy. IHC, 10xpositive staining for (d) SARS-CoV-2 virus, (e) hematoxylin-eosin, (f) anti-isotype staining. Case 2: Optical microscopy. IHC,10x positive staining for (g) SARS-CoV-2 virus, (h) hematoxylin-eosin, (i) anti-isotype staining. Case 3: Optical microscopy.IHC, 10x positive staining for (j) SARS-CoV-2 virus, (k) hematoxylin eosin, (l) anti-isotype staining
Case 1: Optical microscopy. Immunohistochemistry (IHC), 10x positive staining for (a) Acute Respiratory SyndromeCoronavirus 2 (SARS-CoV-2) virus, (b) hematoxylin-eosin, (c) anti-isotype staining. Case 1: Optical microscopy. IHC, 10xpositive staining for (d) SARS-CoV-2 virus, (e) hematoxylin-eosin, (f) anti-isotype staining. Case 2: Optical microscopy. IHC,10x positive staining for (g) SARS-CoV-2 virus, (h) hematoxylin-eosin, (i) anti-isotype staining. Case 3: Optical microscopy.IHC, 10x positive staining for (j) SARS-CoV-2 virus, (k) hematoxylin eosin, (l) anti-isotype staining