Nikhil Prasad Fact checked by:Thailand Medical News Nov 13, 2024 1 year, 3 months, 1 day, 3 hours, 26 minutes ago
Medical News: Introduction to the Apelinergic System and COVID-19
The COVID-19 pandemic has brought significant attention to how viruses, like SARS-CoV-2, impact our bodies in surprising and complex ways. One such pathway involves the apelinergic system, which plays a crucial role in maintaining cardiovascular health, fluid balance, and metabolic regulation. This system includes apelin (AP), a hormone that protects the cardiovascular system, elabela (ELA), and their receptor, APJ. Researchers from Wroclaw Medical University and the Regional Center of Transfusion Medicine and Blood Bank in Poland conducted a study to understand how COVID-19 influences this system over time, even after the initial infection has passed. This
Medical News report sheds light on their findings, which suggest that COVID-19 can lead to prolonged disruption in the apelinergic system that may affect long-term health.
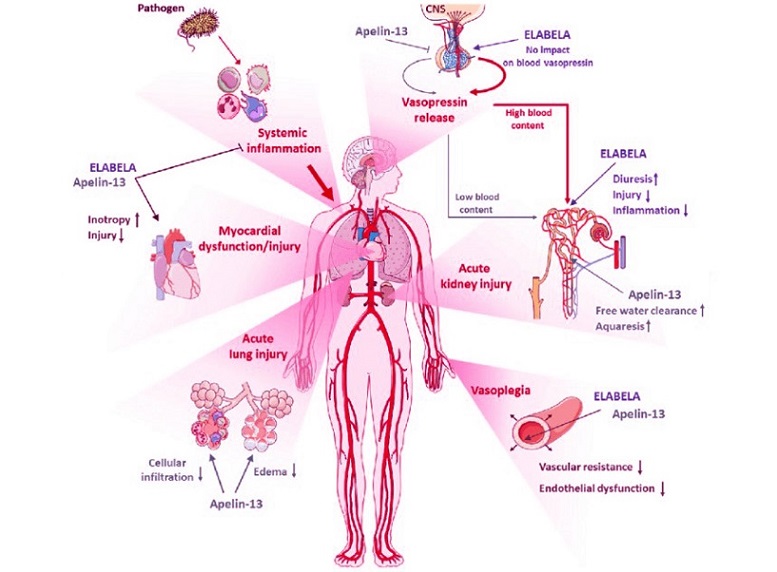
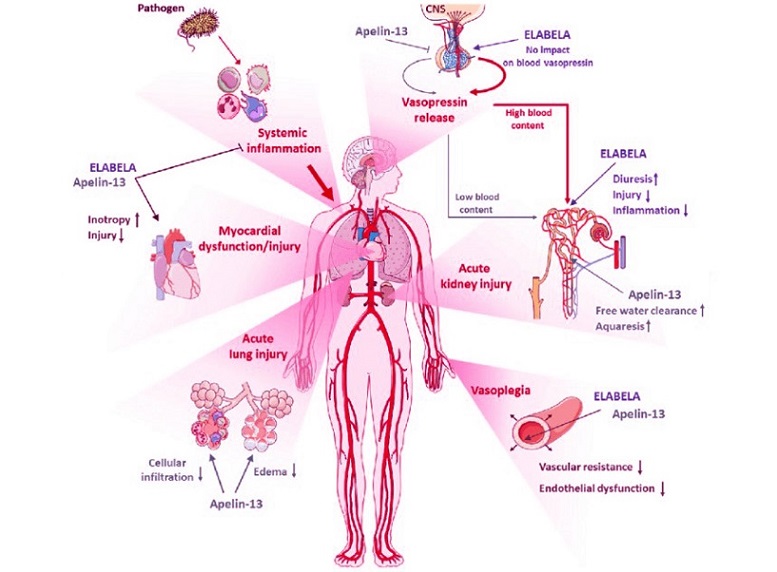 Disruption of the Apelinergic System Can Result In A Wide Array Of Health Issues
The Study Setup: Blood Donors and COVID-19 Recovery
Disruption of the Apelinergic System Can Result In A Wide Array Of Health Issues
The Study Setup: Blood Donors and COVID-19 Recovery
For the study, researchers focused on a unique group: repeat blood donors who had recovered from COVID-19. This group was ideal for investigating changes in the apelinergic system because they tend to be in good health, reducing the likelihood of confounding factors related to chronic health conditions. The research team collected serum samples from 30 repeat donors at four different points in time after their COVID-19 infections: within 60 days, 61-90 days, 91-120 days, and beyond 120 days post-infection. These results were compared to samples from individuals who had donated blood before the pandemic, ensuring they had no exposure to the virus.
Key Findings on Apelin (AP), Elabela (ELA), and APJ Levels
The study's findings reveal fascinating insights into how COVID-19 disrupts the apelinergic system over time. At the outset, it was evident that the concentrations of AP, ELA, and APJ in those who had recovered from COVID-19 were lower than in the uninfected control group. This disruption indicates that the body’s ability to maintain cardiovascular balance may be compromised even months after recovering from COVID-19.
Apelin (AP) and Elabela (ELA) Levels Over Time
In the period shortly after ‘COVID-19 recovery ‘(up to 60 days), levels of both AP and ELA were significantly lower than in the control group. However, these levels showed a gradual increase as more time passed. By the fourth period, beyond 120 days after infection, AP levels had almost returned to normal. Nevertheless, ELA levels, while increased, still did not match those of the control group. The slow recovery in these hormone levels suggests that the apelinergic system struggles to return to a pre-COVID-19 state, which may have implications for long-term cardiovascular and metabolic health.
APJ Receptor: A Prolonged Decrease
The APJ receptor showed the most prolonged effect. Its concentration decreased significantly, reaching its lowest point in the 61-90 day period after infection. Although the
re was some recovery in APJ levels by the fourth period, they remained considerably lower than in the control group. Since APJ plays a vital role in allowing AP and ELA to exert their beneficial effects on the cardiovascular system, this persistent downregulation may have implications for the heart and blood vessels long after the acute phase of COVID-19 has ended.
Understanding the Impact of Apelinergic System Disruption
The apelinergic system interacts closely with the renin-angiotensin-aldosterone system (RAAS), another hormonal system critical for regulating blood pressure and fluid balance. ACE2, the enzyme SARS-CoV-2 binds to for cell entry, usually plays a role in balancing the effects of RAAS. When ACE2 is inhibited by the virus, RAAS activity goes unchecked, leading to increased blood pressure and inflammation. This interaction further disrupts the apelinergic system by reducing the available ACE2, which the body typically relies on for processing apelin peptides.
Studies prior to this have suggested that COVID-19 patients, particularly those with conditions like hypertension or obesity, tend to have lower levels of AP, which could worsen their symptoms. By comparing recovered COVID-19 patients with healthy individuals, this study found a similar pattern: AP levels dropped after infection but began to rise slowly as more time passed. The gradual recovery in AP levels may help explain why some COVID-19 patients eventually experience improvements in their symptoms, although the lower APJ levels suggest that full recovery of the apelinergic system might be challenging.
Elabela’s Role in Cardiovascular Health
While AP has been studied more extensively, ELA is a newer player in the apelinergic system with its own important functions, particularly in cardiovascular health. Initially discovered as essential for heart development in embryos, ELA has since been linked to maintaining healthy blood pressure and vascular integrity in adults. In this study, ELA levels dropped significantly after COVID-19 infection, mirroring the trends seen in AP and highlighting that the virus disrupts multiple components of the apelinergic system.
Implications for COVID-19 Patients and Those with Pre-existing Conditions
The persistent downregulation of the APJ receptor in COVID-19-recovered patients could hold clues to understanding why some people experience prolonged symptoms, commonly known as “long COVID.” The lower levels of AP and ELA post-infection suggest that the body’s natural protective mechanisms may be compromised, particularly in terms of cardiovascular health. For those with pre-existing cardiovascular or metabolic conditions, the lingering effects on the apelinergic system could increase their vulnerability to further health complications.
Given these findings, it’s possible that therapies targeting the apelinergic system could help mitigate some of the long-term effects of COVID-19. For instance, AP-based treatments might be developed to boost the cardiovascular system’s resilience, especially in patients with underlying health risks. However, as AP may also increase susceptibility to SARS-CoV-2 by elevating ACE2 levels, such therapies would need to be administered cautiously and likely only after the virus has been cleared from the body.
Other Studies on the Apelinergic System and COVID-19
This research aligns with previous studies that observed lower AP levels in COVID-19 patients, especially among those with hypertension and obesity. Some researchers have suggested that this apelinergic disruption could partly explain why COVID-19 patients with these pre-existing conditions often fare worse. Others, however, have reported contrasting results, noting increased AP levels in COVID-19 patients. These inconsistencies highlight the need for further research to fully understand the relationship between COVID-19 and the apelinergic system.
Conclusion: A Path Forward
In conclusion, this study sheds light on how COVID-19 affects the apelinergic system over a prolonged period. The gradual but incomplete recovery of AP and ELA levels, combined with the persistent decrease in the APJ receptor, indicates that COVID-19 may have lasting impacts on cardiovascular health. This article underscores the importance of monitoring and potentially supporting the apelinergic system in individuals recovering from COVID-19, particularly those with existing heart or metabolic conditions.
Future research should aim to clarify the exact role of the apelinergic system in post-COVID-19 recovery and to develop targeted treatments that could mitigate the long-term effects of the virus. The findings of this study open up new avenues for understanding COVID-19’s impact on cardiovascular health and for developing potential therapies that support the body’s natural protective systems.
The study findings were published in the peer-reviewed journal: Biomedicines.
https://www.mdpi.com/2227-9059/12/11/2583
For the latest COVID-19 News, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/covid-19-infection-and-vaccination-causes-small-fiber-neuropathy
https://www.thailandmedical.news/news/covid-19-causes-alpha-synucleinopathies
https://www.thailandmedical.news/news/study-reveals-that-covid-19-alters-key-human-genes