BREAKING NEWS! Alarming Surge in Giant Cell Arteritis Cases Raises Concerns of COVID-19 Link!
Thailand Medical - COVID-19 - Giant Cell Arteritis Jul 03, 2023 2 years, 7 months, 1 week, 3 days, 14 hours, 43 minutes ago
British Physicians Found That In The First Wave Of The COVID-19 Pandemic There Was A 118% Increase In GCA Cases Which Are Still Rising Exponentially!
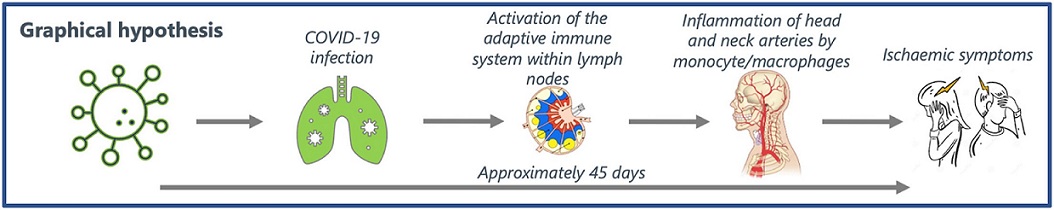
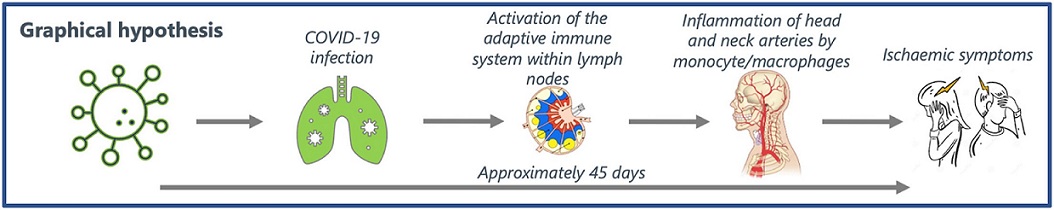
Study Shows That Giant Cell Arteritis (GCA) Can Manifest Between 45 days After COVID-19 Infection!
Thailand Medical: In a recent study conducted at the Royal National Hospital for Rheumatic Diseases (RNHRD) in Bath, UK, physicians have identified a significant increase in giant cell arteritis (GCA) diagnoses following the first wave of the COVID-19 pandemic and subsequent waves. This finding has sparked discussions about a potential connection between COVID-19 and the development of GCA, shedding new light on the causes of this debilitating condition. Improved understanding of the relationship between the virus and GCA may lead to enhanced diagnostic and treatment strategies, ultimately benefiting patients worldwide.
Giant cell arteritis (GCA), also known as temporal arteritis, is a form of vasculitis characterized by inflammation of blood vessels, particularly the arteries in the scalp and head, including those over the temples.
The primary symptom of GCA is typically a new headache, commonly felt around the temples, although it can occur in other areas as well. Additional symptoms may include fatigue, loss of appetite, weight loss, and a flu-like sensation. Jaw pain during chewing can also be experienced. In some cases, GCA can affect the blood supply to the eyes, potentially leading to vision problems. Prompt treatment can help prevent permanent vision loss, making it crucial for patients with active or inactive polymyalgia rheumatica (PMR) to report any new headache, changes in vision, or jaw pain to their healthcare providers.
Diagnosing GCA is not straightforward and does not rely solely on a single blood test. The erythrocyte sedimentation rate (sed rate) is a commonly used blood test that measures inflammation levels, but a high sed rate alone is not sufficient evidence for a GCA diagnosis. In certain cases, an ultrasound of the temporal arteries may be performed. However, a biopsy of the temporal artery is often necessary to confirm the diagnosis.
Overall, GCA is a condition characterized by inflammation of blood vessels, primarily affecting the arteries in the head and scalp. Recognizing the symptoms and seeking appropriate medical attention is crucial for timely diagnosis and treatment to prevent potential complications, including permanent vision loss.
The study aimed to assess the local incidence of GCA during the early stages of the COVID-19 pandemic, specifically from 2020 to 2021, and compare it to pre-pandemic data from 2015 to 2019. Furthermore, researchers sought to examine the temporal relationship between COVID-19 infections and GCA diagnoses to determine if there was a connection between the two.
The study team calculated the annual incidence rates of GCA between 2015 and 2021. They estimated the local prevalence of COVID-19 by analyzing the number of hospital beds occupied by COVID-19-positive patients. By employing Poisson statistics, they compared the average annual incidence of GCA between 2019 and 2020. Additionally, they used Granger causal
ity testing to explore the temporal relationship between COVID-19 prevalence and GCA incidence.
The results were striking. In 2020, there were 60 GCA diagnoses (with a 95% confidence interval of 46-77), compared to 28 diagnoses (CI 19-41) in 2019 (P = 0.016). The peaks in COVID-19 inpatients were found to correlate with peaks in GCA diagnoses. Through Granger causality testing, the researchers discovered a statistically significant association between these peaks, with a lag period of 40-45 days.
The incidence of GCA in Bath experienced a significant increase in 2020 and 2021 compared to the years from 2015 to 2019. The lag period between the peaks of COVID-19 cases and GCA diagnoses suggests that the COVID-19 virus might act as a precipitating factor for GCA. To delve deeper into the causal relationship between these two conditions, further research is underway.
Giant cell arteritis, a form of large vessel vasculitis, predominantly affects individuals over the age of 50. Delayed diagnosis and treatment initiation can result in severe complications, including irreversible visual loss. Despite its prevalence, the exact causes of GCA remain elusive. Some researchers propose an infectious origin, wherein the immune system becomes sensitized, leading to an autoimmune response against antigens within the arteries. Previous studies have already indicated a heightened risk of developing GCA following certain infections, particularly viral upper respiratory tract infections. Expanding our knowledge of the connection between infection and the subsequent development of GCA offers opportunities for improved risk assessment, disease recognition, and therapeutic options.
Corresponding author, Dr Ben Mulhearn from the Royal National Hospital for Rheumatic Diseases told
Thailand Medical News, “The implications of this study are significant. The incidence of GCA in Bath demonstrated a substantial rise in the pandemic years of 2020 and 2021 compared to the non-pandemic years from 2015 to 2019. This finding aligns with similar studies conducted by other groups, reinforcing the notion that the widespread infection of a population with the COVID-19 virus might act as a precipitating factor, similar to upper respiratory tract infections. Scandinavian research has revealed a seasonal pattern in GCA prevalence, with higher rates observed in spring and summer, potentially indicating a role for prior winter infections. However, a multinational meta-analysis conducted in Australia and New Zealand contradicts this seasonal effect, highlighting the importance of considering geographical variations in cyclical infection patterns. Additionally, the similarity in the clinical presentation of COVID-19 and GCA may have contributed to an increased rate of GCA diagnoses during the pandemic.”
The Granger causality test, despite questions regarding its validity, has established a temporal association between COVID-19 prevalence and GCA diagnosis, with a lag period of 40-45 days. It is essential to note, however, that this test alone cannot establish causality, despite its name. Intriguingly, although not statistically significant, a weak association between community COVID-19 prevalence and GCA diagnoses was observed within a broader range of 30-50 days. This raises the possibility of inter-individual variability in the latent period between infection and the onset of autoimmune disease.
Researchers have excluded infections occurring within 30 days of GCA diagnosis to minimize classification bias due to similar presenting symptoms.
One potential mechanism worth exploring is the impact of the virus on endothelial dysfunction. COVID-19 utilizes the angiotensin-converting enzyme 2 (ACE2) receptor, which is highly expressed on vascular endothelium, to enter cells. Endothelial dysfunction can also be influenced by sun exposure, leading to the disruption of the internal elastic lamina. Such disruption, occurring adjacent to the arterial wall's adventitia, may release damage-associated molecular patterns (DAMPs), activating adventitial dendritic cells and priming naïve T cells toward T helper cell type 1 (Th1) and Th17 immunity. Both Th1 and Th17 responses are recognized as critical in initiating autoimmunity. Consequently, the release of chemokines from Th1 and Th17 cells within arterial walls recruits monocytes that differentiate into macrophages, ultimately leading to the characteristic granulomatous lesions observed in GCA.
The study findings now link GCA, an autoimmune disease with an enigmatic origin to the COVID-19 pandemic. This study establishes an association between the two conditions on a population level, with a lag period of 40-45 days, providing further evidence in support of the viral hypothesis of GCA development.
Future investigations aim to delve into this relationship on an individual patient level, utilizing national databases. Understanding the risk factors associated with GCA will enable earlier diagnosis and the mitigation of its serious complications.
The study findings were published in the peer reviewed journal: Heliyon Open Access.
https://www.cell.com/heliyon/fulltext/S2405-8440(23)05107-1
For the latest Medical News, keep on logging to
Thailand Medical News.