Study Uncovers How Hypertension Causes Vascular Dementia Via Reduced Cerebral Blood Flow
Thailand Medical News Team Aug 14, 2023 2 years, 5 months, 4 weeks, 2 days, 18 hours, 12 minutes ago
Thailand Medical: Vascular dementia, a devastating cognitive condition marked by reduced blood flow to the brain, has long eluded effective treatment. However, a new study conducted at the Geoffrey Jefferson Brain Research Centre at the University of Manchester-United Kingdom, has unveiled a potential breakthrough in understanding the root cause of vascular dementia and offers a novel avenue for drug development. The research sheds light on the intricate interplay between high blood pressure and the deterioration of brain arteries, ultimately leading to the development of this debilitating condition.
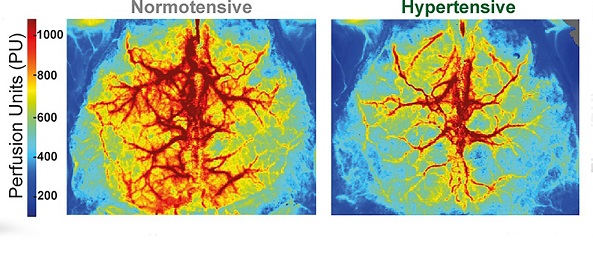
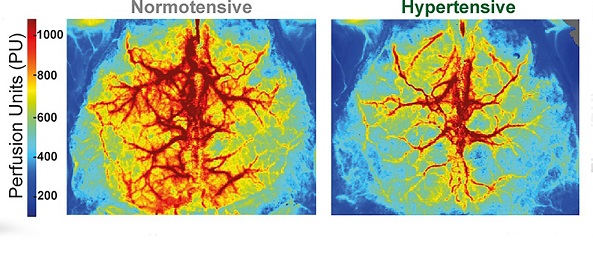 Hypertensive mice display a vascular dementia phenotype. Laser speckle images showing the average perfusion of the dorsal surface of the brain from normotensive (Left) and hypertensive (Right) mice over a 5-min period.
Hypertensive mice display a vascular dementia phenotype. Laser speckle images showing the average perfusion of the dorsal surface of the brain from normotensive (Left) and hypertensive (Right) mice over a 5-min period.
Vascular dementia, the second-most common form of dementia, arises primarily from hypertension-induced damage to cerebral blood vessels, resulting in poor blood circulation to vital brain regions. This deficiency in blood supply deprives brain cells of essential nutrients, leading to their gradual degeneration and demise. Manifesting as symptoms like energy loss, impaired concentration, and memory decline, vascular dementia imposes a significant burden on affected individuals and their families.
A key revelation from this study is the discovery of how persistent high blood pressure disrupts crucial communication processes within artery cells in the brain, triggering a cascade of events that contribute to vascular dementia. While the natural response of brain arteries to fluctuating blood pressure involves periodic narrowing and widening, chronic hypertension distorts this mechanism, causing arteries to remain constricted and impeding blood flow. The underlying mechanisms behind this phenomenon were previously unknown.
Innovative research using mouse models in this study has now illuminated this intricate process. The study reveals that high blood pressure instigates the separation of essential cellular structures responsible for transmitting messages that prompt artery dilation. Using myography, electrophysiology, and Ca2+ imaging, the study team found that the increased constriction was due to separation of the sarcoplasmic reticulum from the plasma membrane in vascular smooth muscle cells, which prevented vasodilatory Ca2+ signals from activating large-conductance K+ channels. The study team proposes that restoring this coupling could improve CBF and slow disease progression.
The potential implications of these findings are monumental. By identifying drugs capable of restoring the disrupted communication within artery cells, researchers hope to rejuvenate blood supply to the brain, thereby slowing down the progression of vascular dementia. Although the study's findings are yet to be verified in human subjects, the fundamental processes of artery constriction and dilation share remarkable similarities between mice and humans.
This promising insight has prompted further investigations into drug candidates that can reinstate the disrupted signaling, potentially leading to clinical trials aimed at revitalizing healthy blood flow in individuals afflicted by vascular dementia.
Professor Dr Adam Greenstein, a distinguished clinician scientist spec
ializing in high blood pressure at the University of Manchester and a lead researcher of the study, emphasized the profound significance of these findings and told
Thailand Medical News, "Our research uncovers a new avenue for drug discovery that may pave the way for the first-ever treatment for vascular dementia. Restoring normal blood flow to damaged brain regions is vital in halting the progression of this devastating condition.”
He added, “Moreover, the potential applications of such drugs extend beyond vascular dementia, offering a potentially novel approach to treating Alzheimer's disease, another neurodegenerative disorder with similar vascular damage.”
Professor Sir Nilesh Samani, the Medical Director at the British Heart Foundation, stressed the urgent need for innovative solutions in tackling vascular dementia, a condition affecting a growing number of individuals. "This exciting research reveals a specific mechanism by which high blood pressure might increase the risk of vascular dementia," he noted. The identification of this mechanism offers a new avenue for therapeutic interventions, igniting hopes that effective treatments could soon emerge to alleviate the suffering of individuals battling this relentless ailment.
The study's profound impact becomes even clearer upon delving into the intricate cellular processes that underpin the development of vascular dementia. Through meticulous experimentation, the researchers elucidated the role of Ca2+ sparks, transient intracellular calcium signals originating from the sarcoplasmic reticulum (SR), in regulating vasodilation. Activation of large-conductance Ca2+-activated K+ (BK) channels on the plasma membrane by these Ca2+ sparks triggers hyperpolarization and vasodilation, vital mechanisms in maintaining healthy blood flow.
The study focused on the BPH/2 mouse model, a polygenic representation of hypertension, as it mirrors key aspects of vascular dementia observed in humans. At the age of eight months, these hypertensive mice demonstrated reduced cerebral blood flow and cognitive impairment, effectively replicating the human experience of vascular dementia. The researchers pinpointed a significant contributing factor to the enhanced constriction of pial arteries, the small cerebral resistance arteries that play a critical role in regulating blood flow across the brain's surface.
It is worth noting that while this study was conducted in mice, the fundamental principles of blood vessel dynamics and response to hypertension are remarkably similar between mice and humans. Thus, the discoveries made in this study could serve as a stepping stone for future human trials, with the ultimate aim of devising targeted therapeutic interventions to restore healthy brain blood flow in individuals afflicted by vascular dementia.
As the research community harnesses the knowledge gained from this groundbreaking study, there is renewed optimism in the field of dementia research. The identification of a specific mechanism by which high blood pressure contributes to vascular dementia not only offers hope for future treatments but also highlights the intricate interconnectedness of vascular health and cognitive well-being. With further exploration and validation, the potential to unravel the complexities of vascular dementia and develop effective drug treatments may finally be within reach, offering a lifeline to the countless individuals and families impacted by this debilitating condition.
The study findings were published in the peer reviewed journal: Proceedings of the National Academy of Sciences.
https://www.pnas.org/doi/10.1073/pnas.2307513120
For the latest COVID-19 News, keep on logging to
Thailand Medical News