Disturbed Monocyte Populations May Be Driving Long COVID Symptoms Like Brain Fog and Fatigue
Nikhil Prasad Fact checked by:Thailand Medical News Team Jun 09, 2025 8 months, 4 days, 23 hours, 49 minutes ago
Medical News: German Scientists Uncover How Changes in Immune Cells Could Be Fueling Long COVID
A team of German researchers has uncovered disturbing immune system abnormalities in people suffering from Long COVID, also known as post-acute sequelae of SARS-CoV-2 infection (PACS). Their findings may help explain why many continue to struggle with chronic symptoms like brain fog, fatigue, and shortness of breath—even years after recovering from the initial infection.
 Disturbed Monocyte Populations May Be Driving Long COVID Symptoms Like Brain Fog and Fatigue
Disturbed Monocyte Populations May Be Driving Long COVID Symptoms Like Brain Fog and Fatigue
The research was conducted by scientists from several top German institutions including the Laboratory for Experimental Transfusion Medicine at Technische Universität Dresden, the German Red Cross Blood Donation Service North-East, the University Hospital Carl Gustav Carus, and the Brandenburgische Technische Universität Cottbus-Senftenberg. In this
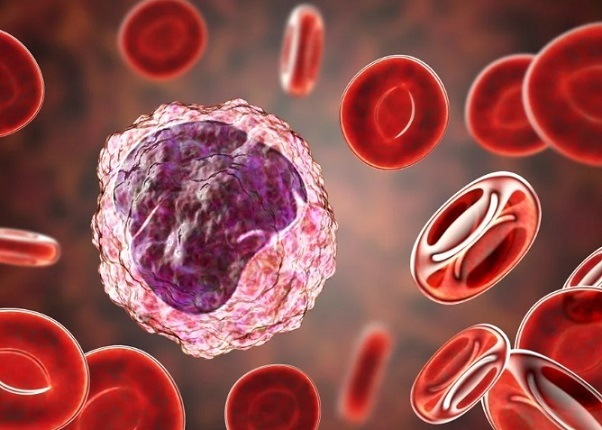
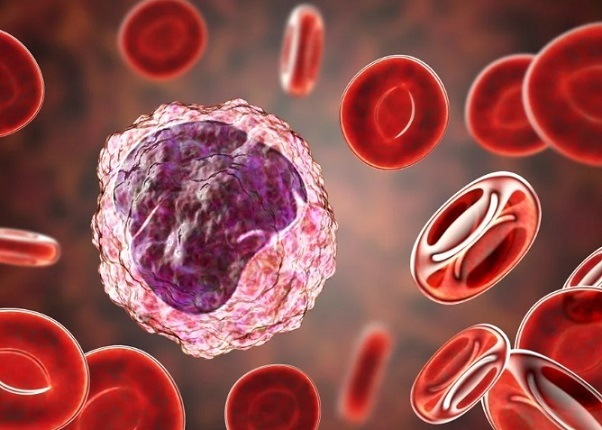
Medical News report, we delve into how specific white blood cells called monocytes—vital players in the body’s immune defense—appear to remain in a dysfunctional state in Long COVID patients, potentially triggering ongoing inflammation and damage.
What the Study Found About the Immune System in Long COVID
The study analyzed blood samples from 32 Long COVID patients and compared them to 22 healthy individuals. Researchers focused on monocytes, which are key immune cells that come in three subtypes: classical, intermediate, and non-classical. These cells help fight infections and regulate inflammation.
Although the total number of monocytes in Long COVID patients was similar to healthy individuals, there were some striking differences. The researchers found significantly increased numbers of intermediate monocytes and a rare, inflammation-prone subtype known as CD56+ monocytes in Long COVID patients. These changes were seen across nearly all participants, regardless of whether they reported fatigue, cough, or breathing issues.
However, the team made an especially notable discovery in those suffering from brain fog. Patients with cognitive problems had significantly higher levels of non-classical monocytes—cells known for patrolling blood vessels and participating in immune surveillance of the brain. This may help explain the neurological symptoms seen in many Long COVID sufferers.
Additionally, these same patients had elevated levels of D-dimer, a blood marker often associated with clotting and inflammation. D-dimer levels have previously been linked to memory and thinking problems in elderly people, suggesting a similar mechanism might be at play in Long COVID.
Signs of a Deep and Lasting Immune Imbalance
Intermediate monocytes—known to produce high levels of inflammatory molecules—are commonly seen in diseases like sepsis and rheumatoid arthritis. Their persistent presence in Long COVID patients, even those sick for over two years, suggests that the immune system remains in a state of low-grade infl
ammation long after the virus is gone.
The CD56+ monocytes, which were also elevated, are not only involved in inflammation but have been previously linked to aging and autoimmune diseases. Worryingly, this increase was found even in younger Long COVID patients, hinting at premature immune aging caused by the virus.
Together, the expansion of intermediate and CD56+ monocytes, along with abnormal non-classical monocytes in patients with brain fog, paints a picture of an immune system stuck in overdrive. The researchers believe this dysregulated monocyte landscape could be playing a central role in sustaining Long COVID symptoms by promoting persistent inflammation, clotting issues, and possibly even infiltration of immune cells into the brain and lungs.
Conclusion
This new research highlights how SARS-CoV-2 may leave behind long-term immune scars in a subset of people, pushing their monocyte system out of balance. The increase in inflammation-prone monocyte subsets—especially in patients experiencing brain fog—suggests that the immune system may be locked into a chronic inflammatory state. These lingering immune shifts may not only explain many Long COVID symptoms but also open the door to potential new treatments targeting these specific immune cells. The fact that these changes persist even two years post-infection underscores the urgent need for more long-term care strategies and diagnostic tools to address the complexities of Long COVID.
The study findings were published in the peer reviewed journal: Frontiers in Immunology.
https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1613034/full
For the latest on Long COVID, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/covid-19-makes-monocytes-dysfunctional-post-infection-raising-risk-of-opportunistic-infections-or-pathogen-reactivation
https://www.thailandmedical.news/news/hyperactivated-killer-t-cells-and-il-3-found-to-be-driving-long-covid-symptoms
https://www.thailandmedical.news/news/ongoing-breathing-issues-in-long-covid-might-be-tied-to-iga-autoimmunity-and-hidden-clotting-dysfunction
https://www.thailandmedical.news/articles/long-covid
https://www.thailandmedical.news/pages/thailand_doctors_listings