Persistent Glial Activation and Blood Brain Barrier Damage Could Explain Long COVID Neurological Symptoms
Nikhil Prasad Fact checked by:Thailand Medical News Team Oct 29, 2025 3 months, 2 weeks, 2 days, 1 hour, 30 minutes ago
Medical News: Emerging Clues About How COVID-19 Impacts the Brain
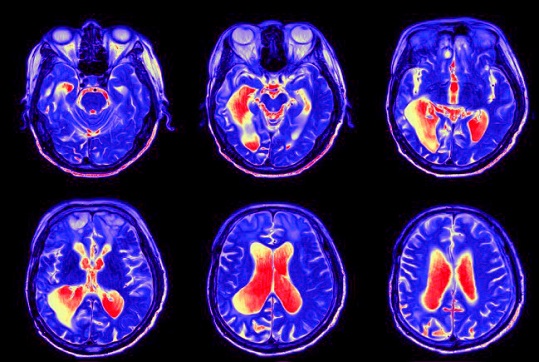
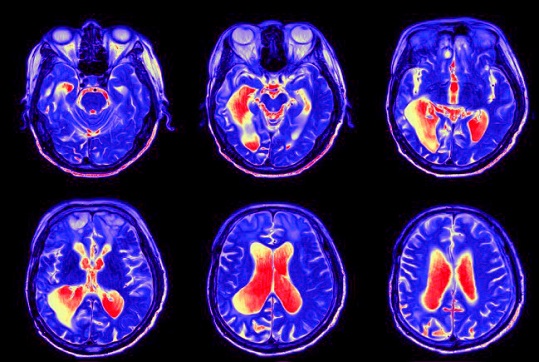
Researchers from the University of Iowa’s Carver College of Medicine have released a comprehensive review exploring how SARS-CoV-2 affects the brain and nervous system. The study reveals that the neurological complications linked to both acute COVID-19 and long COVID are more likely caused by chronic immune-driven inflammation and blood–brain barrier (BBB) damage rather than direct viral infection of brain cells. This
Medical News report highlights that persistent glial activation—an immune response by brain support cells—and microvascular injury may explain why many people continue to experience “brain fog,” memory loss, and fatigue months after recovering from the virus.
 Persistent Glial Activation and Blood Brain Barrier Damage Could Explain Long COVID Neurological Symptoms
Inflammation Rather Than Infection Is the Main Driver
Persistent Glial Activation and Blood Brain Barrier Damage Could Explain Long COVID Neurological Symptoms
Inflammation Rather Than Infection Is the Main Driver
According to the Iowa research team, while traces of viral RNA and proteins have been detected in autopsied human brains, they appear in low quantities and are unevenly distributed, suggesting the virus does not replicate significantly in neural tissue. Instead, systemic inflammation triggered by the so-called “cytokine storm” during infection disrupts the integrity of the BBB, allowing immune cells and inflammatory molecules to leak into the brain. This process activates microglia and astrocytes—two key glial cell types that, when chronically stimulated, can cause neuronal damage, impaired signaling, and lasting cognitive dysfunction. Animal studies confirm that even after the virus is cleared from the body, the brain remains inflamed and structurally altered for weeks to months, mirroring the human long COVID experience.
Animal and Human Evidence Paint a Unified Picture
Postmortem studies of COVID-19 victims consistently show cerebrovascular damage, microhemorrhages, and hypoxic injury. Similar findings in non-human primates and mice demonstrate that viral infection indirectly injures the brain through inflammation, coagulation, and endothelial dysfunction. Experiments using transgenic mice that express human ACE2 receptors reveal that SARS-CoV-2 can access the brain through the olfactory pathway but does not spread widely, while other models show pronounced BBB disruption and vascular inflammation without extensive neuronal infection. The convergence of evidence indicates that it is the immune system’s overreaction—not direct viral attack—that destabilizes brain homeostasis.
Glial Cells and the Blood Brain Barrier Hold the Key
The review underscores that persistent activation of microglia and astrocytes, combined with damaged blood vessels, may be the underlying cause of long-term neurological symptoms. These include cognitive decline, sleep disturbances, and mood disorders that linger for months or even years. Elevated levels of inflammatory cytokines such as IL-6, TNF-α, and CXCL10 in cerebrospinal fluid further su
pport this link. Researchers emphasize that controlling chronic neuroinflammation and restoring BBB integrity could be crucial therapeutic targets for long COVID.
Why These Findings Matter for Long COVID Patients
The study provides a framework for understanding why some individuals experience lasting brain-related symptoms despite testing negative for the virus. By comparing autopsy data, imaging results, and animal experiments, the scientists conclude that persistent glial activation and neurovascular inflammation form the biological basis for post-acute neurological syndromes. They warn that elderly individuals and those with diabetes or preexisting brain conditions may face higher risks of long-term damage due to heightened inflammatory responses. Future treatments may need to focus on anti-inflammatory agents that specifically protect the BBB and normalize glial function.
Persistent glial activation and BBB disruption, rather than viral persistence, now appear to be central to how COVID-19 reshapes the brain. As long COVID continues to affect millions globally, understanding these processes could lead to more effective therapies to prevent chronic neurological decline and improve quality of life for survivors.
The study findings were published in the peer reviewed journal: Viruses.
https://www.mdpi.com/1999-4915/17/11/1432
For the latest on long COVID, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/articles/long-covid