COVID-19 News: Study Shows That SARS-CoV-2 Infections Can Cause Acute Phrenic Neuropathy and Diaphragmatic Dysfunction!
COVID-19 News - Acute Phrenic Neuropathy - Diaphragmatic Dysfunction Mar 12, 2023 2 years, 11 months, 1 week, 5 days, 21 hours, 2 minutes ago
COVID-19 News: A new study by researchers from Angeles Mocel Hospital-Mexico, IMSS Venados Hospital-Mexico and National Institute of Respiratory Diseases-Mexico has found that SARS-CoV-2 infections can cause acute phrenic neuropathy and diaphragmatic dysfunction and presented 4 cases studies to substantiate their claims.
Acute Phrenic Neuropathy is a condition characterized by nerve damage affecting the phrenic nerve, which is the nerve that controls the contraction of the diaphragm, the main muscle involved in breathing. This condition can result in diaphragmatic paralysis or weakness, leading to respiratory failure and the need for mechanical ventilation. Acute Phrenic Neuropathy can be caused by a variety of factors, including viral infections or autoimmune disorders. Symptoms of this condition can include shortness of breath, difficulty breathing, and fatigue. Treatment may involve medications to address the underlying cause, respiratory support, and physical therapy to rehabilitate the diaphragm.
Already a previous
COVID-19 News coverages had shown that even asymptomatic or mild SARS-CoV-2 infections can lead to diaphragm damage.
https://www.thailandmedical.news/news/even-asymptomatic-and-mild-covid-19-causes-neuromuscular-damage-to-the-diaphragm-resulting-in-the-long-covid-manifestations-of-fatigue-and-dyspnea
Apart from respiratory symptoms, COVID-19 has been associated with several neurological manifestations, including neuropathies. Neuropathy is a rare neurological manifestation of COVID-19 and can lead to significant acute consequences that may increase mortality.
The study team presented a case series of four Mexican patients diagnosed with diaphragmatic dysfunction due to phrenic neuropathy during acute COVID-19.
Neuropathies associated with COVID-19: SARS-CoV-2 infection can cause several neurological manifestations. Several reports from around the world have described inflammatory olfactory neuropathy, motor peripheral neuropathy, and neuromuscular involvement in critically ill COVID-19 patients. These reports indicate that SARS-CoV-2 can cause damage to the peripheral nervous system. However, the primary cause of hypoxemia in COVID-19 patients is the damage caused by the viral infection in the lung parenchyma.
Diaphragmatic neuropathy in COVID-19 patients: Although there are several reports of neuromuscular disease due to COVID-19, documented cases of diaphragmatic neuropathy are rare. Diaphragmatic neuropathy can cause rapid deterioration of respiratory mechanics in COVID-19 patients
The four patients included in this report were adults with an average age of 60.5 ± 8.5 (range: 52-69 years), with a documented diagnosis of COVID-19 and a severe clinical presentation upon hospital admission. The patients were admitted to two different hospitals in Mexico City between December 2020 and March 2021. During their hospitalization, the patients underwent several evaluations, including nasopharyngeal swab testing for SARS-C
oV-2 with real-time polymerase chain reaction assay (RT-PCR), D-Dimer, ferritin, creatine phosphokinase (CPK), creatine phosphokinase-MB (CPK-MB), Clauss fibrinogen assay (CFA), general blood tests, chest CT, and bilateral nerve conduction velocities (NCV) of the PNs to document neuronal damage. None of the patients had been vaccinated against SARS-CoV-2 at the time of contracting the infection.
Case 1: A 56-year-old man with poorly controlled type 2 diabetes mellitus, systemic arterial hypertension, and obesity grade 1 presented with headache, anosmia, ageusia, non-productive cough, myalgia, and fever. He was admitted to the hospital after 8 days of increasing severity, with low oxygen saturation, high blood pressure, rapid heartbeat, and breathing difficulties. He was diagnosed with SARS-CoV-2 infection and treated with anticoagulant, steroid anti-inflammatory, insulin, and antihypertensive medications. During hospitalization, he developed nerve damage, which was treated with medication and exercise-based pulmonary rehabilitation. He was discharged after 28 days of hospitalization.
Case 2: A 55-year-old woman with poorly controlled type 2 diabetes mellitus and systemic arterial hypertension presented with cough, weakness, and fatigue. She was admitted to the hospital with a high fever and low oxygen saturation, and was diagnosed with SARS-CoV-2 infection. She was treated with anticoagulants, anti-inflammatory steroids, insulin, and antihypertensive and ascorbic acid medication. Despite treatment, she experienced respiratory failure and required advanced airway management. She developed polyneuropathy and multiple organ failure, leading to her death after 49 days of hospitalization.
Case 3: A 69-year-old woman with poorly controlled type 2 diabetes mellitus, systemic arterial hypertension, and hypothyroidism was initially treated for diarrhea and fever, but was later admitted to the hospital with low oxygen saturation and a diagnosis of SARS-CoV-2 infection. She was treated with medication, but experienced neurological deterioration and brain damage, as well as sensory-motor peripheral polyneuropathy. She received physical therapy and rehabilitation, including swallowing rehabilitation and supramaximal electrostimulation, and was discharged after 58 days of hospitalization.
Case 4: A 52-year-old man with no significant medical history was diagnosed with SARS-CoV-2 infection and was hospitalized after developing respiratory failure. He experienced neurological complications, including abdominal myoclonus, which affected his breathing. He received treatment with medication and physical rehabilitation, including electrostimulation of the phrenic nerve and diaphragmatic rehabilitation. He was discharged after 67 days of hospitalization, having made significant progress in his neurological condition and breathing stability.
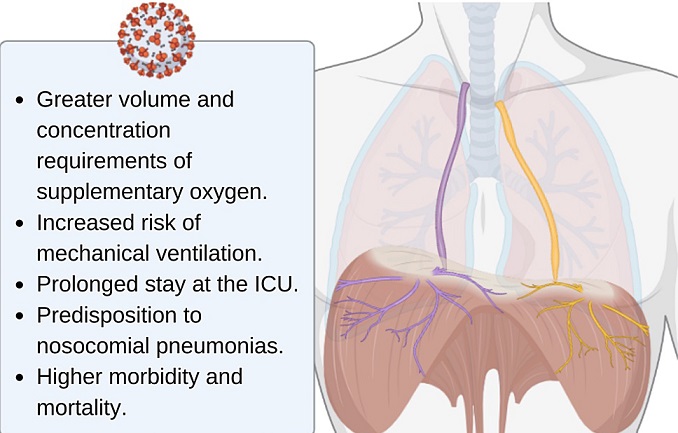
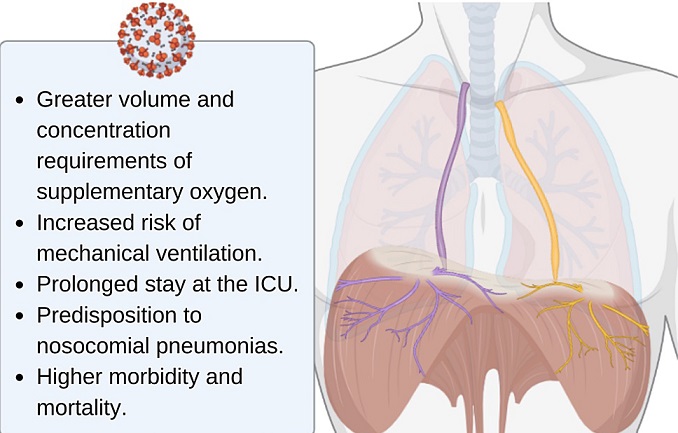
Conclusion: COVID-19 patients with phrenic nerve neuropathy represent a therapeutic challenge due to their high oxygen requirements, caused by the malfunction of ventilatory mechanics secondary to neuromuscular damage and the damage that pneumonia generates in lung tissue. This case series confirms and extends the neurological manifestations of COVID-19, highlighting the impact on the neuromuscular dysfunction of the diaphragm and its consequences, such as the difficulty of weaning from mechanical ventilation. The findings suggests that SARS-CoV-2 may be a causal factor of acute phrenic neuropathy and diaphragmatic dysfunction.
Clinicians should be aware of the possibility of diaphragmatic neuropathy in COVID-19 patients, especially those with severe clinical presentations. Further studies are necessary to determine the prevalence and pathophysiology of diaphragmatic neuropathy in COVID-19 patients.
Limitations of this report include the absence of diaphragmatic ultrasound studies and the extensive information on neurological complications due to COVID-19.
The study findings were published in the journal: Cureus.
https://www.cureus.com/articles/134941-acute-phrenic-neuropathy-and-diaphragmatic-dysfunction-as-a-complication-of-covid-19-a-report-of-four-cases#!/
For the latest
COVID-19 News, keep on logging to Thailand Medical News.