Unraveling the Intricacies Of Blood Clotting In COVID-19: How SARS-CoV-2 Spurs A Hypofibrinolytic State
COVID-19 News: Hypofibrinolytic State May 24, 2023 2 years, 8 months, 3 weeks, 8 minutes ago
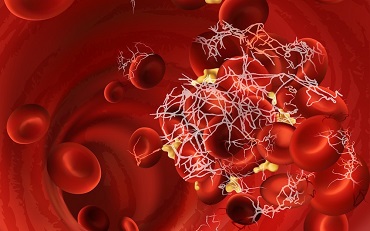
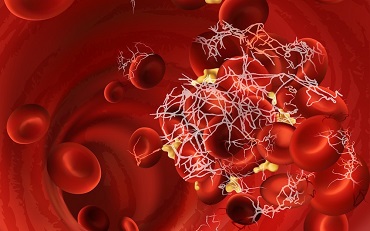
COVID-19 News: In the midst of the ongoing COVID-19 pandemic, researchers from Johns Hopkins University School of Medicine in Baltimore, Maryland-USA, have uncovered a puzzling aspect of the disease: patients infected with the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) show signs of coagulation activation and an increased risk of thrombosis, yet they do not typically develop a consumption coagulopathy - a condition where clotting factors are rapidly depleted. Furthermore, despite elevated levels of D-dimers, indicating fibrin degradation, these patients exhibit a hypofibrinolytic state characterized by impaired clot breakdown. This perplexing paradox has led scientists on a quest to understand the underlying mechanisms of the coagulopathy associated with COVID-19.
To shed light on this enigma, the study team conducted a comprehensive study involving 64 adult patients with SARS-CoV-2 infection, including 36 with moderate symptoms and 28 with severe symptoms. They compared these individuals to a control group of 16 uninfected individuals. The focus of their investigation was on plasma protease inhibitors….specifically, serpins, Kunitz, Kazal, and Cystatin-like inhibitors that target the fibrinolytic system. The study team examined various inhibitors, such as Plasminogen Activator Inhibitor-1 (PAI-1), Tissue Plasminogen Activator/Plasminogen Activator Inhibitor-1 complex (t-PA/PAI-1), Neuroserpin, Protease Nexin-1 (PN-1), and others, to assess their association with disease severity.
The study findings were intriguing. The study team found that while there was no significant reduction in plasma anticoagulants, indicating a compensated state, there was a consistent increase in fibrinolysis inhibitors, including PAI-1, Neuroserpin, PN-1, Plasmin-α2-Antiplasmin Complex, and t-PA/PAI-1. This rise in fibrinolysis inhibitors was associated with moderate and severe disease, suggesting a link between these markers and the severity of COVID-19 symptoms.
To further investigate the role of these inhibitors in the lungs, the study team examined post-mortem lung tissues from eight fatal COVID-19 cases. They discovered a significant overexpression of PAI-1 in epithelial cells, macrophages, and endothelial cells, while Neuroserpin was primarily found in intra-alveolar macrophages.
Corresponding author, Dr Ivo M. B. Francischetti from the Department of Pathology, Johns Hopkins University School of Medicine, told
COVID-19 News reporters from TMN, “These study findings indicated a high anti-fibrinolytic activity in the lungs, potentially contributing to a local and systemic hypofibrinolytic state that predisposes patients to thrombosis and other complications associated with COVID-19.”
The study team also delved into the complex interplay between coagulation and complement activation in COVID-19. They found that the lungs play a central role in this process through the expression of tissue factor (TF), the loss of anticoagulants, neutrophil extracellular trap (NET) formation, and complement activation. These pro-thrombotic events are further influenced by elements of Virchow's triad - hypercoagulability, endothelial dysfunction, and blood stasis, which increase the risk of thrombosis.
Despite these factors, the study team observed that most patients did not develop consumption coagulopathy, indicating a compensated disseminated intravascular coagulation (DIC) state rather than acute DIC typically seen in sepsis.
One of the intriguing findings was the dysregulation of fibrinolysis in COVID-19. Despite the presence of high D-dimer levels, indicating increased fibrin formation and breakdown, there is often an imbalance favoring fibrin formation and reduced fibrinolysis in COVID-19 patients. This dysregulation of fibrinolysis contributes to the development of microvascular thrombosis and is associated with poor clinical outcomes.
Several mechanisms have been proposed to explain the dysregulation of fibrinolysis in COVID-19. One key factor is the increased expression of plasminogen activator inhibitor-1 (PAI-1), the primary inhibitor of fibrinolysis. PAI-1 inhibits the conversion of plasminogen to plasmin, which is responsible for fibrin breakdown. Elevated levels of PAI-1 in COVID-19 patients inhibit fibrinolysis, leading to the accumulation of fibrin in blood vessels.
Additionally, endothelial dysfunction plays a significant role in fibrinolysis dysregulation. The endothelium, which lines the blood vessels, normally maintains a balance between procoagulant and anticoagulant factors. In COVID-19, the virus directly infects endothelial cells, causing endothelial dysfunction and disrupting this delicate balance. The damaged endothelium releases procoagulant factors, such as von Willebrand factor (vWF), which promotes platelet aggregation and thrombus formation, while also reducing the production of anticoagulant factors, including tissue plasminogen activator (tPA), which promotes fibrinolysis.
Furthermore, the excessive inflammation seen in COVID-19 contributes to fibrinolysis dysregulation. Inflammatory cytokines, such as interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-alpha), can upregulate PAI-1 production and inhibit fibrinolysis. The systemic inflammation observed in severe COVID-19 cases perpetuates this dysregulated fibrinolysis state.
The dysregulation of fibrinolysis in COVID-19 has important clinical implications. It contributes to the formation of blood clots, particularly in the small blood vessels of the lungs, leading to pulmonary microvascular thrombosis. This thrombotic burden can result in acute respiratory distress syndrome (ARDS) and other severe complications.
To address the dysregulated fibrinolysis in COVID-19, various treatment approaches have been explored. Anticoagulant therapies, such as low molecular weight heparin, have been used to prevent and treat thrombotic events. Fibrinolytic agents, such as recombinant tPA, have also been considered to promote fibrin breakdown. However, the optimal management of fibrinolysis dysregulation in COVID-19 is still an area of active research.
In summary, dysregulation of fibrinolysis in COVID-19 is characterized by an imbalance favoring fibrin formation and reduced fibrinolysis, primarily driven by elevated PAI-1 levels, endothelial dysfunction, and excessive inflammation. This dysregulated state contributes to the development of microvascular thrombosis and worsens clinical outcomes. Further understanding of the mechanisms underlying fibrinolysis dysregulation in COVID-19 is crucial for the development of targeted therapies to mitigate thrombotic complications and improve patient outcomes.
The study findings were published in the peer reviewed journal: eJHAem (A journal of the British Society for Haematology- Wiley)
https://onlinelibrary.wiley.com/doi/10.1002/jha2.654
For the latest
COVID-19 News, keep on logging to Thailand Medical News.