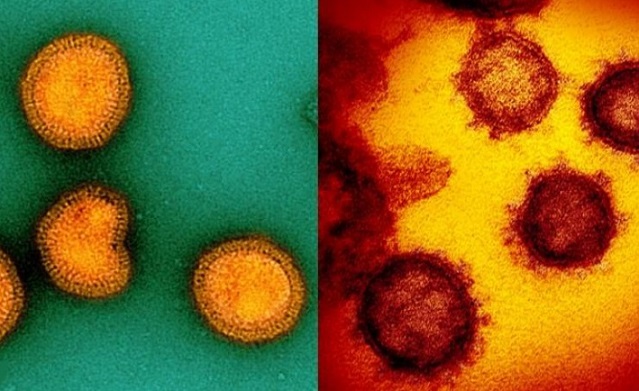
Scientists Discover How SARS-CoV-2 and Influenza Viruses Hijack Human Cells by Rewiring Sugar Metabolism
Nikhil Prasad Fact checked by:Thailand Medical News Team Jun 16, 2025 8 months, 1 week, 23 hours, 16 minutes ago
Medical News:
Breakthrough study reveals how viruses manipulate a key enzyme to supercharge replication and worsen inflammation.
A major new study by scientists from The University of Hong Kong, Guangzhou Medical University, Southern Medical University, and Huazhong Agricultural University has uncovered a hidden biological mechanism that both SARS-CoV-2 and Influenza viruses exploit to spread quickly and cause severe inflammation in the human body. The research identifies a cellular enzyme called PFKFB3 as the critical switch that viruses turn on to boost their own replication and at the same time ignite harmful inflammatory responses.
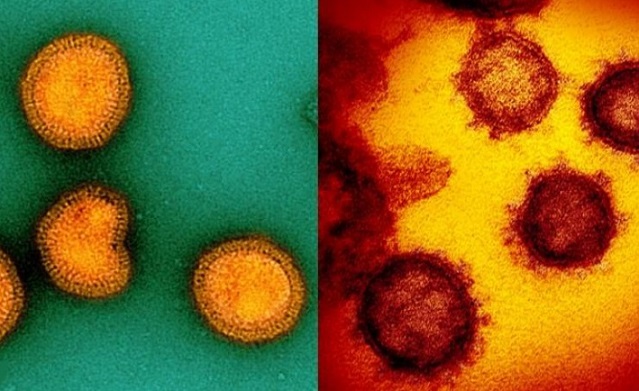 Scientists Discover How SARS-CoV-2 and Influenza Viruses Hijack Human Cells by Rewiring Sugar Metabolism
Scientists Discover How SARS-CoV-2 and Influenza Viruses Hijack Human Cells by Rewiring Sugar Metabolism
This
Medical News report explains how these viruses manipulate human metabolism to their advantage, making it harder to treat infections once symptoms have already started. The scientists found that both SARS-CoV-2 and Influenza A viruses produce proteins that chemically modify the host enzyme PFKFB3 in a way called SUMOylation. This modification activates the enzyme, which in turn fuels a sugar-burning process known as glycolysis. While glycolysis normally provides cells with energy, the virus uses it to rapidly multiply and spread.
One Enzyme Powers Two Deadly Processes
PFKFB3 does more than just help viruses replicate. The same process also leads to the production of a molecule called bradykinin—a chemical that can cause dangerous inflammation. The study showed that when PFKFB3 is activated by viral proteins, it increases levels of fructose 2,6-bisphosphate, which not only boosts glycolysis but also triggers kallikrein enzymes to release bradykinin. This chain reaction causes a “double strike”: higher virus loads and stronger inflammatory damage.
Researchers observed that patients hospitalized with influenza had significantly higher levels of bradykinin in their blood. In laboratory models, mice lacking PFKFB3 in their lungs were far more resistant to both influenza and SARS-CoV-2 infections. Not only did they show lower viral loads, but they also experienced less lung damage and inflammation.
A New Class of Antivirals May Be on the Horizon
The scientists tested a drug called AZ-67, which specifically blocks PFKFB3. In mice infected with Influenza A virus, this treatment—even when started two days after infection—offered far better survival compared to standard antiviral drug oseltamivir (Tamiflu). Mice treated with AZ-67 showed lower viral counts, reduced bradykinin and IL-1β levels (a key inflammation marker), and healthier lung tissue.
These results are important because many people with respiratory virus infections only seek medical help after symptoms worsen, making early treatment difficult. A drug like AZ-67 could extend the treatment window, targeting both viral replication and the harmful inflammation it causes.
Bradykinin&a
mp;rsquo;s Surprising Role in Helping Viruses Enter Cells
Another startling finding is how bradykinin may actually help viruses like SARS-CoV-2 enter human cells. The study found that PFKFB3-driven increases in bradykinin also boost the glycosylation of ACE2—the cellular receptor the virus uses to gain entry. This helps the virus stick more easily to cells and penetrate them.
When scientists blocked bradykinin receptors or the enzymes that produce it, they observed a significant drop in viral entry. This points to another potential treatment strategy: targeting the bradykinin system to prevent both infection and inflammation.
Conclusion
The research offers powerful insights into how viruses like SARS-CoV-2 and Influenza hijack our body’s energy systems to their benefit. By rewiring glycolysis through PFKFB3 and manipulating bradykinin levels, they create the perfect storm—rapid replication and destructive inflammation. Targeting this metabolic axis may offer a game-changing strategy for treating respiratory viruses, especially in patients who cannot access care early. The study paves the way for new broad-spectrum antivirals that go beyond killing the virus—they also protect the body from the damage it leaves behind.
The study findings were published on a preprint server and are currently being peer reviewed.
https://www.researchsquare.com/article/rs-6694201/v1
For the latest COVID-19 News, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/hungarian-researchers-discover-that-viruses-hijack-ancient-dna-loops-to-control-human-genes-and-trigger-disease
https://www.thailandmedical.news/news/aryl-hydrocarbon-receptors-help-rna-viruses-including-sars-cov-2-and-hiv-evade-the-immune-system
https://www.thailandmedical.news/news/israeli-study-finds-that-immunity-gene-ceacam1-shows-potential-against-respiratory-viruses-including-hmpv