Glaucoma News: Meta Study Finds That Glaucoma Patients Have Higher Serum Uric Acid Levels!
Nikhil Prasad Fact checked by:Thailand Medical News Team Oct 22, 2023 2 years, 3 months, 3 weeks, 2 days ago
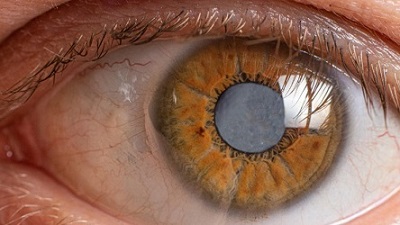
Glaucoma News: Glaucoma, a silent thief of sight, is the leading cause of irreversible blindness worldwide. The prevalence of this condition is on the rise, and it is predicted that over 110 million people will be afflicted by glaucoma by the year 2040. Glaucoma typically progresses silently in its early stages, with symptoms often remaining unnoticed by patients. However, if left untreated, it can lead to irreversible blindness, making early diagnosis and treatment critical.
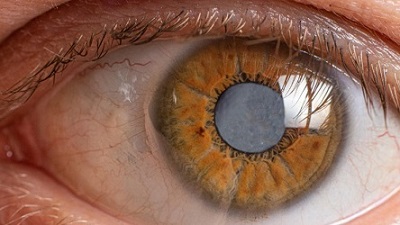
Detecting glaucoma early is challenging, primarily due to its asymptomatic nature, resulting in a significant number of undiagnosed cases. Intraocular pressure (IOP) measurement is a cornerstone of glaucoma diagnosis and management, as elevated IOP is a major risk factor for the condition. While elevated IOP can cause glaucomatous optic neuropathy, some patients with glaucoma exhibit normal IOP levels, suggesting the involvement of other factors in the disease's pathogenesis.
Glaucoma is traditionally considered an eye disease, but emerging research has linked it to central nervous system degeneration. This neurodegenerative process leads to gradual optic nerve degeneration and the loss of retinal ganglion cells, which is the primary cause of vision loss in glaucoma. Despite extensive research, the exact pathogenesis of glaucomatous optic neuropathy remains elusive.
Uric acid (UA), a metabolite of purine, is present in intracellular and body fluids. It is known to possess both pro-oxidant and antioxidant properties, playing a vital role in the regulation of reactive oxygen species. UA has demonstrated its potential as a protective factor in other neurodegenerative conditions like Parkinson's disease, Huntington's disease, Alzheimer's disease, and amyotrophic lateral sclerosis. However, the role of UA in the development of glaucoma remains unclear.
This
Glaucoma News report delves into a systematic review and meta-analysis, conducted to provide insight into the relationship between serum UA levels and glaucoma, shedding light on the potential role of UA as a biomarker in glaucoma research.
The Meta-Analysis
The meta-analysis conducted by researchers from Shahid Sadoughi University of Medical Sciences in Iran, Tehran University of Medical Sciences in Iran, Assil Gaur Eye Institute in California, and Shiraz University of Medical Sciences in Iran aimed to evaluate the association between serum UA levels and glaucoma. By analyzing the available case-control studies, the researchers sought to determine whether there was a significant connection between UA levels and glaucoma.
Methodology
The researchers systematically searched multiple databases, including PubMed, Scopus, Web of Science, and Google Scholar, until November 20, 2022, to identify relevant case-control studies comparing the serum UA concentrations of patients with glaucoma and control groups. The analysis used the mean ± standard deviation difference to assess the variation in serum UA levels between glaucoma patients and control subjects.
Results
Six case-control studies, involving a total of 1,221 gl
aucoma patients and 1,342 control subjects, were included in the meta-analysis. The analysis employed a random-effects model, which revealed that the mean UA level in glaucoma patients was 0.13 higher than in control subjects, though this difference was not statistically significant. The high level of heterogeneity in the results indicated that the findings from these studies varied considerably.
Discussion
The findings of this meta-analysis indicate that glaucoma patients tend to have higher serum UA levels compared to control subjects, but this difference is not statistically significant. This intriguing discovery is essential, as it highlights the need for further research into the potential association between elevated UA levels and glaucoma pathogenesis.
While the exact cause of glaucoma remains unknown, there are several theories and contributing factors that researchers have explored over the years. One prevailing theory suggests that oxidative stress and neuroinflammation play a significant role in glaucomatous optic neuropathy. Antioxidants have been shown to have potential protective effects in glaucoma by lowering IOP, promoting vascular health, and preventing retinal ganglion cell loss.
Uric acid, a key antioxidant in the body, has been reported to contribute significantly to the overall antioxidant capacity of plasma. Animal studies and clinical trials have suggested that higher serum UA concentrations can help prevent neuronal degeneration. Notably, studies have indicated that a lower baseline serum UA concentration is associated with a higher risk of primary angle-closure glaucoma (PACG) progression.
On the other hand, some studies have suggested that systemic inflammation is related to glaucomatous damage. This idea is supported by findings that glaucoma patients often have higher bacterial oral counts, and low-dose lipopolysaccharide administration in glaucoma animal models leads to neuronal loss and axonal degeneration. Recent studies have also reported a significant association between Heliobacter pylori infection and glaucoma.
Collectively, these findings suggest that glaucoma patients may experience an imbalance between antioxidative and oxidative processes in the body. It is possible that elevated serum UA levels could be consumed by reacting with oxidative agents in the body. Previous studies have indeed reported that individuals with higher UA levels have a reduced risk of glaucoma and that UA levels are inversely related to glaucoma severity.
However, one study that compared serum UA levels between pseudoexfoliation patients (a leading cause of secondary glaucoma) and controls found no significant difference in UA levels between the two groups. This discrepancy suggests that the association between UA levels and glaucoma may not be uniform across all glaucoma subtypes.
Moreover, studies have reported elevated UA levels in the aqueous humor of some glaucoma patients. This observation raises the possibility that oxidative stress could contribute to trabecular meshwork cell apoptosis and extracellular matrix accumulation, leading to increased resistance in the aqueous humor outflow pathway and elevated IOP. Therefore, elevated serum UA levels might impair the trabecular meshwork's physiology, ultimately contributing to glaucomatous optic neuropathy.
However, it is essential to recognize that IOP elevation alone does not provide a comprehensive understanding of glaucoma pathophysiology. Other risk factors, particularly vascular impairment in the optic nerve and surrounding tissues, have also been suggested. Clinical and experimental research suggests that UA-induced inflammatory responses and oxidative stress can contribute to microvascular impairments, possibly via detrimental effects on the endothelium.
Several in vitro and in vivo studies have indicated that UA may lead to endothelial dysfunction, which is associated with open-angle glaucoma. Additionally, studies have reported that elevated UA levels are independently linked to choroidal and retinal microcirculation impairment. Higher serum UA concentrations have been associated with decreased retinal capillary plexus vessel density, suggesting a harmful impact on the retinal microvasculature.
Interestingly, chronic renal disease has also been significantly associated with an increased risk of developing glaucoma. Elevated UA levels have been implicated in the pathogenesis of chronic renal disease, leading to higher glomerular blood pressure. Given the structural similarities between the choroid plexus in the human eye and the renal glomerulus, it is possible that UA's role in glaucoma development mirrors its impact on chronic renal disease.
In conclusion, this meta-analysis presents a significant body of evidence from case-control studies on the association between serum UA levels and glaucoma. While the findings suggest that serum UA concentrations tend to be higher in glaucoma patients than in controls, this association is not statistically significant. However, it is essential to note that this study does not establish a causal relationship between UA and glaucoma.
The study findings were published in the peer reviewed journal: Frontiers in Medicine.
https://www.frontiersin.org/articles/10.3389/fmed.2023.1159316/full
For the latest
Glaucoma News, keep on logging to Thailand Medical News.