Doctors Warn That COVID-19 Vaccines Can trigger Rare Skin Disease Called Sneddon-Wilkinson Disease in Some
Nikhil Prasad Fact checked by:Thailand Medical News Team Jun 16, 2025 8 months, 1 week, 1 day, 22 hours, 49 minutes ago
Medical News: An Unusual Case Links COVID-19 Vaccine to Sneddon Wilkinson Disease
In an intriguing medical twist, doctors in China have reported a rare skin condition triggered by a COVID-19 vaccine. A young woman developed Sneddon–Wilkinson disease (SWD), a little-known but painful skin disorder, after receiving a third dose of an inactivated SARS-CoV-2 vaccine. The case, documented by Dr. Riqu Cao and Dr. Tianhong Xu from the Department of Dermatology at Hangzhou Third People’s Hospital in Zhejiang, adds to the growing evidence of unexpected skin reactions following COVID-19 vaccinations.
 Doctors Warn That COVID-19 Vaccines Can trigger Rare Skin Disease Called Sneddon-Wilkinson Disease in Some
Doctors Warn That COVID-19 Vaccines Can trigger Rare Skin Disease Called Sneddon-Wilkinson Disease in Some
Sneddon–Wilkinson disease, also known as subcorneal pustular dermatosis, is an inflammatory skin disorder marked by pustule-filled rashes mainly in the folds of the body like the groin, underarms, and elbows. It is considered a form of neutrophilic dermatosis, which means it involves an overactivity of certain white blood cells in the skin. This
Medical News report highlights the unusual and unexplained nature of this condition when it occurs following vaccination, raising questions about immune system reactions in certain individuals.
A Delayed Reaction with Increasing Severity
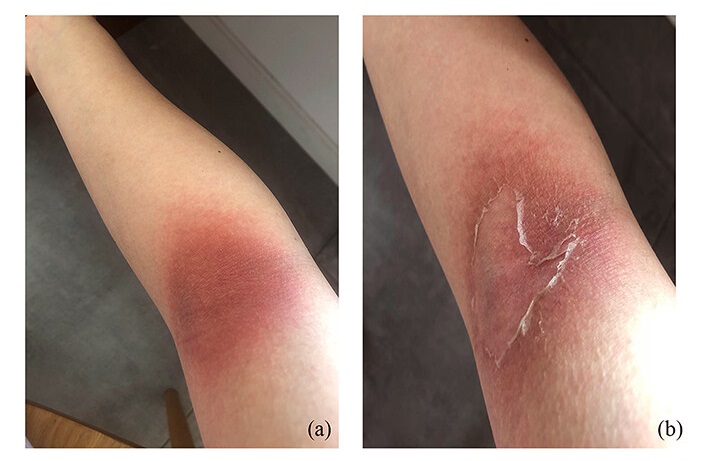
The 29-year-old woman began experiencing mild symptoms just eight days after receiving her booster shot of an inactivated COVID-19 vaccine. Initially, she developed dry and peeling skin, which she assumed was a minor irritation. But over the next few weeks, her condition worsened. She developed red, itchy plaques that eventually formed crusty lesions in sensitive areas such as her groin, elbow folds, and around the belly button.
Notably, she had previously experienced mild skin irritation after her earlier vaccine doses, but the symptoms had gone away on their own. This time, however, the rash persisted and spread, prompting her to seek medical help. Doctors observed distinct scaly lesions with a darker center and red outer ring—classic signs of SWD. A skin biopsy confirmed the diagnosis, revealing clusters of neutrophils (a type of immune cell) gathered just beneath the top layer of skin, creating pustule-like formations.
Successful Treatment with Herbal-Based Medication
The medical team prescribed compound glycyrrhizin, a treatment derived from licorice root known for its anti-inflammatory and immune-modulating properties. Over a two-month course, her symptoms fully resolved, leaving only mild skin discoloration. Remarkably, she remained symptom-free for two years without relapse.
Laboratory tests ruled out other common causes of such skin reactions, including autoimmune diseases and bacterial infections. All antibody tests for conditions like pemphigus and pemphigoid came back negative, strengthening the case that her symptoms were indeed linked to the vaccine.
Possible Mechanism Behind the Skin Reaction
While SWD&rsquo
;s exact causes remain a mystery, it is often associated with other underlying illnesses such as multiple myeloma or certain infections. However, in this patient, no such underlying issues were found. Instead, researchers suspect that the vaccine may have triggered the condition by interacting with specific receptors in the skin known as ACE2 receptors. These receptors are also the gateway that the actual SARS-CoV-2 virus uses to enter cells. Skin cells called keratinocytes have a high concentration of these ACE2 receptors, making them potential targets for both the virus and the vaccine’s mimicking components.
When these skin cells are stimulated—either by the virus or vaccine—they can release chemical signals that summon white blood cells like neutrophils to the area, potentially leading to the kind of skin inflammation seen in SWD.
There have also been other skin conditions linked to COVID-19 vaccines, including Sweet syndrome, facial pustular eruptions, and new-onset pustular psoriasis. This further supports the theory that in some individuals, the vaccine may cause an overactive immune response in the skin.
Conclusions and Public Health Implications
While this case remains rare, it serves as a critical reminder that vaccines, though overwhelmingly safe and beneficial, can trigger unexpected immune responses in isolated individuals. The patient’s condition improved with a simple and safe treatment, and she has not experienced any flare-ups since. Although this does not undermine the value of COVID-19 vaccines, it does underscore the need for continued monitoring of post-vaccination symptoms, especially skin-related ones.
Doctors should remain vigilant for unusual dermatological symptoms following vaccinations and should consider SWD in differential diagnoses if similar presentations occur. More research is also needed to understand why some people have these rare reactions and whether genetic or immune system factors are involved. As global vaccination campaigns continue, documenting and understanding these anomalies will be crucial to improving vaccine safety protocols and patient care.
The study findings were published in the peer reviewed journal: Clinical Cosmetic and Investigational Dermatology
https://www.tandfonline.com/doi/full/10.2147/CCID.S524100
For the latest on COVID-19 Vaccines, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/illinois-study-finds-that-covid-19-vaccines-do-not-prevent-long-covid-neurological-issues
https://www.thailandmedical.news/news/covid-19-mrna-jabs-can-cause-new-onset-of-acute-interstitial-nephritis
https://www.thailandmedical.news/news/breaking-covid-19-news-doctors-in-thailand-warn-that-covid-19-vaccines-could-possibly-lead-to-tumor-expansion-in-certain-cancers
https://www.thailandmedical.news/articles/vaccine-news