Brazilian Research Uncovers The Role of TIGIT+ T Regulatory Cell Subset In COVID-19 Severity, Nosocomial Infections And Fatal Outcomes
Thailand Medical News Team Aug 27, 2023 2 years, 5 months, 3 weeks, 6 days, 16 hours, 38 minutes ago
COVID-19 Research: The emergence of the COVID-19 pandemic presented a formidable challenge to healthcare systems worldwide, with a significant portion of infected individuals requiring mechanical ventilation for severe respiratory distress. While the advent of COVID-19 vaccines has alleviated some aspects of the pandemic, severe cases leading to fatal outcomes remain a concern. Besides the direct impact of the virus, nosocomial infections acquired during hospitalization further complicate the prognosis, with sepsis being a leading cause of death in intensive care units (ICUs). As such, an in-depth understanding of the immune response in COVID-19 patients is imperative for effectively managing the disease, preventing respiratory failure, and countering nosocomial infections.
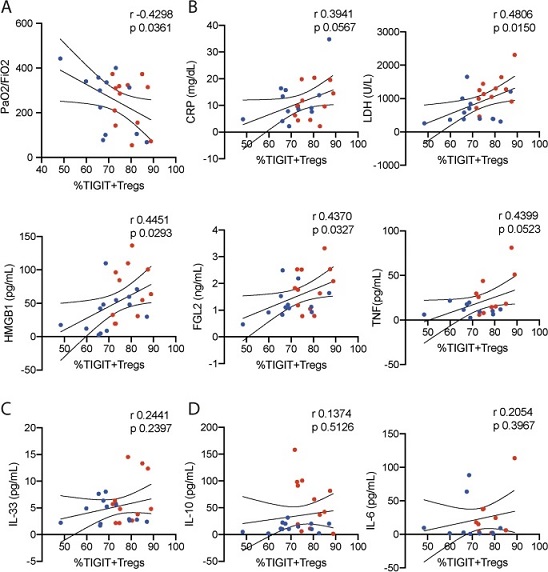
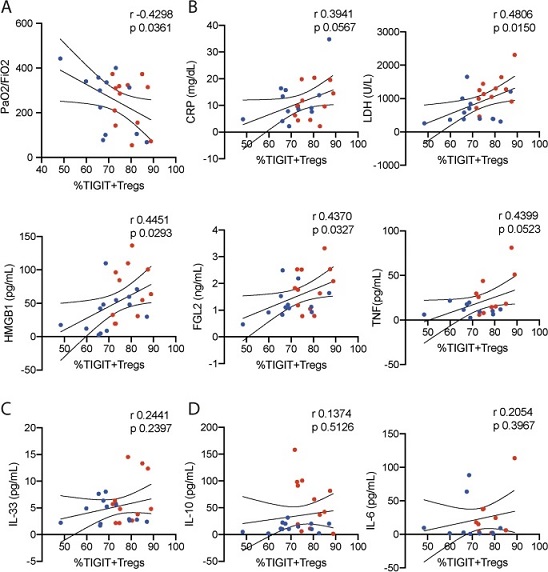 The prevalence of the TIGIT+Tregs correlates with lung dysfunction and increased inflammation. Correlation between the frequency of TIGIT+Treg subset among the FOXP3+Treg repertoire and the (A) PaO2/FiO2, and the plasmatic levels of (B) CRP, LDH, HMGB1, FGL2, and TNF; (C) IL-33; (D) IL-10 and IL-6. All parameters were analyzed during admission of 26 COVID-19 patients that did require mechanical ventilation during hospitalization. The blue-dots represent the survivors and red-dots is related to non-survivors. Spearman’s rank-order correlation (r) was calculated to describe correlations.
The prevalence of the TIGIT+Tregs correlates with lung dysfunction and increased inflammation. Correlation between the frequency of TIGIT+Treg subset among the FOXP3+Treg repertoire and the (A) PaO2/FiO2, and the plasmatic levels of (B) CRP, LDH, HMGB1, FGL2, and TNF; (C) IL-33; (D) IL-10 and IL-6. All parameters were analyzed during admission of 26 COVID-19 patients that did require mechanical ventilation during hospitalization. The blue-dots represent the survivors and red-dots is related to non-survivors. Spearman’s rank-order correlation (r) was calculated to describe correlations.
The subset of T regulatory cells (Tregs) expressing T cell Ig and ITIM domain receptor (TIGIT) along with FOXP3 is recognized for its pivotal role in maintaining immune homeostasis, self-tolerance, and inflammation control. Nevertheless, recent evidence suggests that this TIGIT+FOXP3+ Treg subset (TIGIT+Tregs) may inadvertently contribute to immune dysfunction.
Notably, these cells have been associated with dampening cellular immunity and rendering septic individuals susceptible to opportunistic infections. Given this, it is plausible that TIGIT+Tregs could significantly impact the severity of COVID-19, potentially aggravating the defense mechanisms against nosocomial infections during hospitalization. Thus, this
COVID-19 Research study by researchers from Ribeirão Preto Medical School, University of São Paulo-Brazil seeks to explore the correlation between TIGIT+Tregs levels and mechanical ventilation requirements, fatal outcomes, and nosocomial infections in COVID-19 patients.
COVID-19 Severity and Immunomodulation
In the initial stages of the pandemic, the need for mechanical ventilation was a critical issue, emphasizing the gravity of severe cases. Although vaccination efforts have curtailed hospitalizations, severe infections persist, necessitating a comprehensive understanding of the immune response. The risk of sepsis is substantially elevated among ICU patients, characterized by a dysregulated immune reaction triggered by infection-induced organ dysfunction. Besides known risk factors such as metabolic disorders and cardiovascular conditions, nosocomial infections have emerged as a major cause of mortality following respiratory failure.
Tregs, primarily characterized by FOXP3 expression, play a crucial role in maintaining immune balance. However, reports indicate that disruption of the Treg repertoire may correlate with COVID-19 severity by curbing antiviral immunity and promoting an excessive inflammatory respo
nse. Of particular interest, TIGIT+Tregs, a subset exerting robust immunosuppressive effects, has been implicated in enhancing susceptibility to opportunistic infections. This study postulates that the expansion of TIGIT+Tregs might intensify COVID-19 severity by undermining defense mechanisms against nosocomial infections during ICU hospitalization.
Exploring the Role of TIGIT+Tregs
To investigate the potential association between TIGIT+Tregs and disease severity, the study conducted an immunophenotyping analysis on blood samples from unvaccinated COVID-19 patients upon hospital admission. The research spanned from May 29th to August 6th, 2020, encompassing 72 patients. Stratification of patients during hospitalization allowed the assessment of TIGIT+Tregs levels concerning mechanical ventilation requirements, fatal outcomes, and nosocomial infections.
The findings unveiled a notable prevalence of TIGIT+Tregs in COVID-19 patients at admission. Strikingly, this subset exhibited a progressive increase in patients requiring mechanical ventilation and those facing fatal outcomes. The prevalence of TIGIT+Tregs was positively correlated with impaired pulmonary function, elevated plasma levels of specific markers (LDH, HMGB1, FGL2, and TNF), and increased inflammation. Furthermore, non-survivors demonstrated higher levels of plasma IL-33, HMGB1, FGL2, IL-10, and IL-6. Alarmingly, bacteremia was observed to be over five times higher in non-survivors compared to survivors.
Discussion: Unraveling the Mechanisms
COVID-19 shares several hallmarks with sepsis, including cytokine storms, tissue damage, and an imbalanced immune response. IL-33, released during tissue damage, fosters TIGIT+Tregs expansion, a phenomenon reminiscent of sepsis-induced immunosuppression. Severe COVID-19 cases were characterized by a cytokine storm, tissue damage, and signs of dysregulated immunity. Notably, decreased levels of IFN-γ, a critical antiviral mediator, were observed in patients requiring mechanical ventilation.
While COVID-19 patients in ICUs exhibited reduced FOXP3+Tregs compared to healthy individuals, the study affirmed that worsening disease severity correlated with heightened FOXP3+Tregs levels. Moreover, the effector/memory phenotype of these cells correlated with inflammation, tissue damage, and lung dysfunction.
Comorbidities like obesity, metabolic syndrome, and diabetes, associated with worse COVID-19 outcomes, were also linked to an expansion of the TIGIT+Tregs subset. This could potentially result from meta-inflammation and its impact on the immune system's response to viral infections.
Implications and Future Directions
The study's outcomes underscore the importance of TIGIT+Tregs in COVID-19 severity, nosocomial infections, and fatal outcomes. The expansion of TIGIT+Tregs during hospitalization aligns with intensified inflammation, lung dysfunction, and bacteremia. Given the parallels between COVID-19 and sepsis, therapeutically controlling tissue damage and inflammation might mitigate TIGIT+Tregs expansion and subsequently reduce susceptibility to nosocomial infections.
Although the study's scope is limited by the absence of post-intervention data and a small patient cohort, the potential of TIGIT blockade to restore TCD8+ cell functions suggest a promising avenue for preventing nosocomial and opportunistic infections. Further investigations are warranted to substantiate these findings and explore the implications of TIGIT modulation in ICU-related diseases beyond COVID-19.
Conclusion
The study's comprehensive analysis sheds light on the pivotal role of TIGIT+Tregs in exacerbating COVID-19 severity, nosocomial infections, and fatal outcomes. The association between TIGIT+Tregs expansion and inflammatory responses, tissue damage, lung dysfunction, and hospital-acquired bacteremia underscores the need for targeted therapeutic interventions. These findings pave the way for further research into immunomodulatory strategies aimed at reducing TIGIT+Tregs-mediated immunosuppression, ultimately improving patient outcomes and combating nosocomial infections in COVID-19 and beyond.
The study findings were published in the peer reviewed journal: Scientific Reports.
https://www.nature.com/articles/s41598-023-39924-7
For the latest
COVID-19 Research, keep on logging to Thailand Medical News.