Nikhil Prasad Fact checked by:Thailand Medical News Team Dec 05, 2025 3 months, 1 day, 16 hours, 25 minutes ago
Medical News: A Powerful New Strategy to Tackle Triple Negative Breast Cancer
Triple-negative breast cancer (TNBC) is one of the deadliest and most treatment-resistant forms of breast cancer. It spreads rapidly, returns quickly after treatment, and lacks the hormone receptors that are usually targeted in other breast cancer therapies. But researchers at the Medical University of South Carolina (MUSC) Hollings Cancer Center may have found a promising solution.
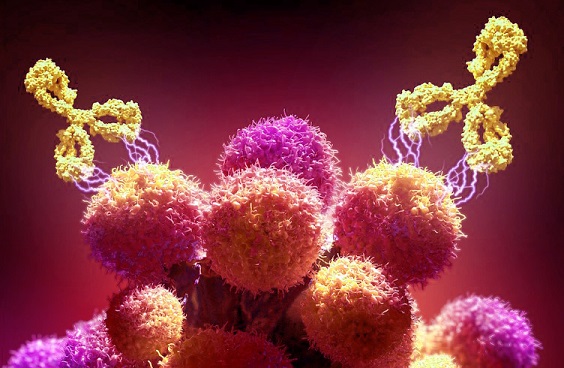
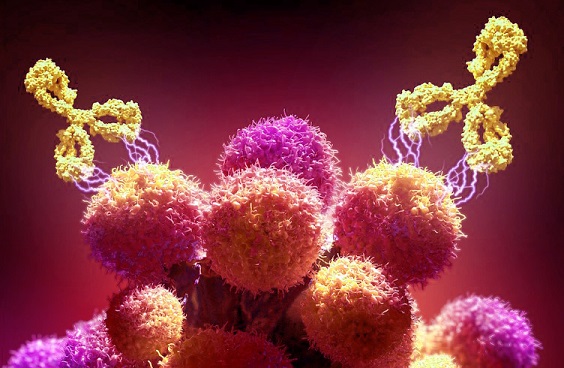 A new antibody therapy shows promise in fighting aggressive triple-negative breast cancer and reversing
A new antibody therapy shows promise in fighting aggressive triple-negative breast cancer and reversing
immune suppression.
This
Medical News report highlights a major scientific development involving a humanized monoclonal antibody that blocks a key protein helping cancer cells grow and evade the immune system. The antibody not only shrinks tumors and prevents cancer spread but also reprograms immune cells to fight cancer more effectively—even in cases where chemotherapy has failed.
Targeting the Root of Cancer Resistance
The research zeroes in on a protein called secreted frizzled-related protein 2 (SFRP2). SFRP2 enables tumors to grow blood vessels, avoid cell death, and suppress immune responses. Previous studies by Dr. Nancy Klauber-DeMore and her team had already identified this protein’s role in breast cancer development, but this new study goes further.
The scientists developed a humanized monoclonal antibody (hSFRP2 mAb) to block SFRP2. In multiple preclinical trials using advanced models of TNBC, the antibody significantly reduced tumor size and metastases, especially to the lungs—a key danger zone for TNBC progression.
Immune Cells Reawakened to Fight Back
One of the most exciting findings is how the antibody reprograms tumor-associated macrophages (TAMs)—immune cells that usually help cancer evade detection. In TNBC, these macrophages typically turn into the M2 type, which protects tumors. However, hSFRP2 mAb pushed them toward the M1 type, which actively attacks tumors by producing interferon-gamma, a powerful immune-boosting molecule.
The antibody also revitalized T-cells, another key immune fighter, which often become “exhausted” and ineffective in TNBC. After treatment with the antibody, T-cells showed renewed activity, suggesting a restored ability to combat the tumor.
Chemotherapy Resistance Overcome
One of the major challenges in TNBC is drug resistance, especially to standard treatments like doxorubicin. In this study, even TNBC cells that had become resistant to doxorubicin were still vulnerable to hSFRP2 mAb. The antibody caused these cells to die off in large numbers, offering hope for patients whose cancers no longer respond to conventional therapies.
Importantly, the antibody avoided healthy tissue and concentrated only in tumor areas, which could mean fewer side effects compared to traditional chemotherapy.
Wider I
mpact Across the Cancer Landscape
Beyond breast cancer, SFRP2 has also been found in other cancers like osteosarcoma, melanoma, pancreatic and kidney cancers. The researchers believe the antibody’s effects could potentially apply to many tumor types. The presence of SFRP2 in both tumor cells and immune cells in the cancer microenvironment makes it an especially promising target for new therapies.
Interestingly, the study also found high levels of CD38—a molecule known to block immune responses—closely aligned with SFRP2 in TNBC tumors. This opens up new questions about whether hSFRP2 mAb could enhance responses to checkpoint inhibitors, another class of immune therapies, by neutralizing both SFRP2 and CD38 effects.
A Step Toward Clinical Trials
While the antibody is not yet approved for human use, it has been licensed to Innova Therapeutics, a Charleston-based biotech firm, which is now raising funds for first-in-human clinical trials. It has already received rare pediatric and orphan disease designations from the U.S. FDA for osteosarcoma, underscoring its potential broader impact.
These findings could represent a new frontier in breast cancer treatment. By offering a therapy that works on multiple levels—shrinking tumors, reversing immune suppression, and overcoming drug resistance—hSFRP2 mAb may soon become a powerful tool against one of the most aggressive cancers known. The targeted approach also reduces side effects, which is a major advantage over existing chemotherapy regimens. If ongoing development and human trials confirm these results, patients with triple-negative breast cancer could finally have access to a treatment that is both effective and less toxic.
The study findings were published in the peer reviewed journal: Breast Cancer Research.
https://link.springer.com/article/10.1186/s13058-025-02176-6
For the latest on Breast Cancer, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/articles/cancer