COVID-19 News: Medical Researchers From Kunming-China Warn That COVID-19 Can Trigger Tumefactive Demyelinating Lesions In Multiple Sclerosis Patients
Nikhil Prasad Fact checked by:Thailand Medical News Team Nov 27, 2023 2 years, 2 months, 4 weeks, 37 minutes ago
COVID-19 News: In the relentless battle against the COVID-19 pandemic, a new frontier of challenges emerges as medical researchers from the Affiliated Hospital of Kunming University of Science and Technology in Wenshan, China, and The First People’s Hospital of Yunnan Province, Kunming, China, report a startling case. A 31-year-old female patient, initially diagnosed with relapsing-remitting multiple sclerosis (RRMS), experienced a transformative journey as tumefactive demyelinating lesions (TDLs) manifested post-infection with SARS-CoV-2. This case covered in this
COVID-19 News report not only highlights the intricate nature of neurological disorders during the pandemic but also underscores the potential contributory role of the virus in triggering or exacerbating demyelinating diseases of the central nervous system (CNS).
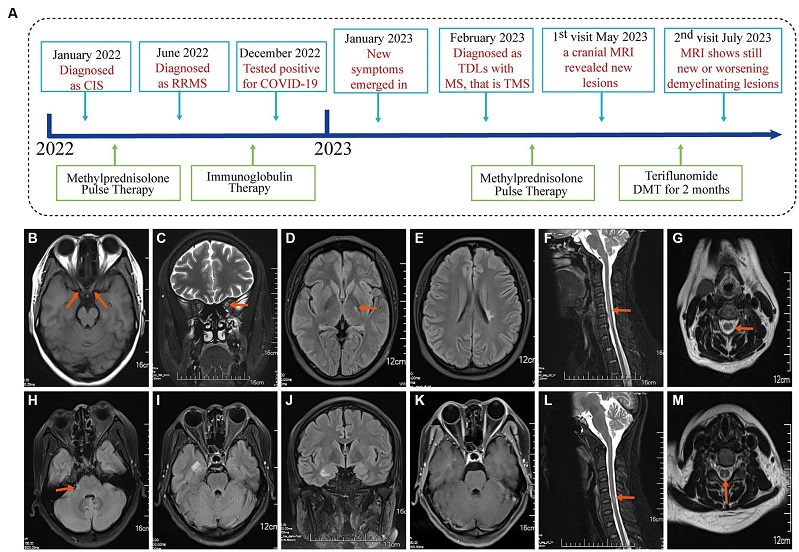
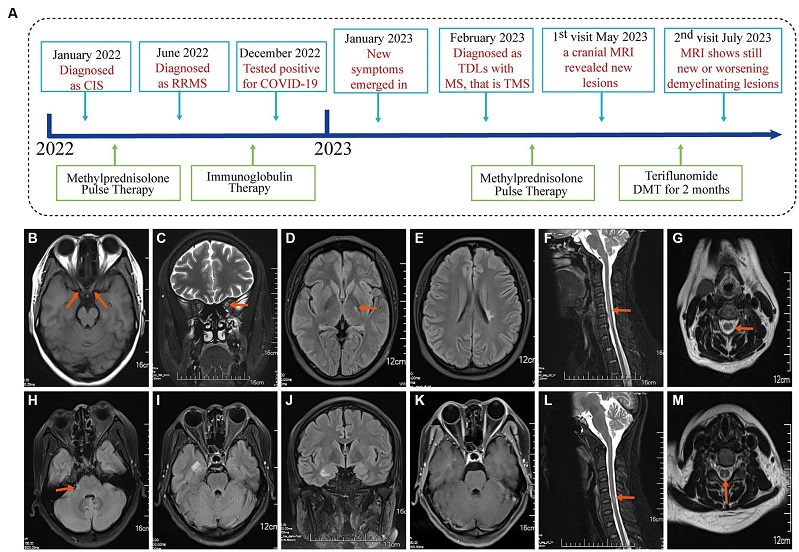 Event timeline for the case and MRI of the brain and spinal cord in January 2022 and June 2022. (A) The timeline showing the relevant events in the case. (B,C) T1WI and T2WI showed bilateral optic nerve enlargement and signal abnormalities. (D,E) The T2Flair displays small lesions located in the left posterior limb of the internal capsule and the cortical spinal tract area near the body of the left lateral ventricle. (F,G) T2WI revealed signal abnormalities in the cervical cord at the C3-6 vertebral plane. Diagnosed as a clinically isolated syndrome. (H–J) MRI of the brain and spinal cord in June 2022 with disease recurrence and T2Flair revealed new small lesions in the right cerebral peduncle, near the temporal horn of the right lateral ventricle, and in the hippocampal region. (K) T1WI-C shows right hippocampal lesion enhancement (active phase) in June 2022. (L,M) T2WI showed cervical spinal cord lesion shrinkage. Diagnosed with relapsing–remitting multiple sclerosis in June 2022.
Multiple Sclerosis: An Overview
Event timeline for the case and MRI of the brain and spinal cord in January 2022 and June 2022. (A) The timeline showing the relevant events in the case. (B,C) T1WI and T2WI showed bilateral optic nerve enlargement and signal abnormalities. (D,E) The T2Flair displays small lesions located in the left posterior limb of the internal capsule and the cortical spinal tract area near the body of the left lateral ventricle. (F,G) T2WI revealed signal abnormalities in the cervical cord at the C3-6 vertebral plane. Diagnosed as a clinically isolated syndrome. (H–J) MRI of the brain and spinal cord in June 2022 with disease recurrence and T2Flair revealed new small lesions in the right cerebral peduncle, near the temporal horn of the right lateral ventricle, and in the hippocampal region. (K) T1WI-C shows right hippocampal lesion enhancement (active phase) in June 2022. (L,M) T2WI showed cervical spinal cord lesion shrinkage. Diagnosed with relapsing–remitting multiple sclerosis in June 2022.
Multiple Sclerosis: An Overview
Multiple Sclerosis (MS) remains an enigmatic autoimmune disease characterized by demyelination in the central nervous system. Despite its rarity in China, with an incidence rate of 0.235 cases per 100,000 people per year from 2016 to 2018, MS globally affects 35.9 cases per 100,000 people. The disease manifests in various clinical phenotypes, including relapsing-remitting MS (RRMS), secondary progressive MS (SPMS), primary progressive MS (PPMS), or progressive-relapsing MS (PRMS). Intriguingly, patients with MS may also develop TDLs, an uncommon form of CNS demyelination associated with autoimmunity. Recent reports suggest a potential link between SARS-CoV-2 infection and the triggering or exacerbation of central nervous system demyelinating diseases, adding complexity to the already challenging landscape of MS diagnosis and treatment.
The Unprecedented Case
The focal point of this study revolves around a 31-year-old female patient whose medical journey began with a diagnosis of RRMS. However, the plot thickened as she subsequently developed TDLs following an infection with SARS-CoV-2. Initial intervention with immunotherapy, specifically glucocorticoid pulses, led to a significant improvement in both clinical and radiological characteristics. However, the patient's trajectory took an unexpec
ted turn after the initiation of disease-modifying therapy (DMT) with teriflunomide. Two months into the DMT treatment, imaging follow-up revealed a deterioration of the patient's condition, challenging the efficacy of teriflunomide in managing TDLs. This unique case not only underscores the complexity and challenges in diagnosing and managing tumefactive inflammatory demyelinating disorders in MS patients amid a SARS-CoV-2 infection but also raises questions about the virus's potential contributory role in CNS demyelination.
Clinical Features and Diagnosis
The patient's medical odyssey began on January 26, 2022, with symptoms of blurred vision leading to admission to the People's Hospital of Wenshan Prefecture. Neurological physical examination revealed reduced vision in both eyes, with a significant decline in the left eye. Optical coherence tomography (OCT), visual evoked potential (VEP), and brainstem auditory evoked potential (BAEP) results were normal. However, MRI examinations of the optic nerve, brain, and spinal cord, along with cerebrospinal fluid (CSF) examination, indicated positive oligoclonal bands, suggestive of clinically isolated syndrome (CIS). Pulse therapy of methylprednisolone sodium succinate led to significant improvement, and the patient was discharged.
Subsequent admissions occurred on June 27, 2022, due to numbness in both lower limbs, and on February 20, 2023, for dizziness and headaches. Imaging revealed an increase in demyelinating lesions in the brain, consistent with RRMS. However, the situation took a more complicated turn during the third admission on February 20, 2023, as the patient presented with memory reduction and enhanced lesions on an enhanced MRI of the brain and spinal cord. CSF analysis indicated blood–brain barrier damage and the presence of CSF-restricted IgG oligoclonal bands, ultimately leading to the diagnosis of TDLs with multiple sclerosis, specifically tumefactive multiple sclerosis (TMS).
Diagnosis and Differential Diagnosis
Adhering to the 2017 McDonald criteria for diagnosing multiple sclerosis, the patient's experience of more than two clinical attacks, along with evidence of more than two lesions, solidified the MS diagnosis. To exclude other potential causes, a comprehensive differential diagnosis was conducted. This involved virus testing, including negative results for serum HIV, CSF toxoplasma antibodies, herpes simplex virus (II) antibodies, rubella virus antibodies, cytomegalovirus antibodies, and EB virus antibodies. Additionally, tests for AQP4, MOG, GFAP, and MBP in both CSF and serum were negative, ruling out NMOSD-related diseases. Normal autoimmune antinuclear antibody and erythrocyte sedimentation rate results excluded autoimmune encephalitis, while serum tumor markers and thoracoabdominal CT excluded paraneoplastic syndrome. The patient's refusal of a brain biopsy limited the differential diagnosis further.
Patient's History of COVID-19 and CNS Impact
The patient received two doses of the inactivated novel Coronavirus vaccine (Vero cell) in June 2021 with no adverse reactions. However, on December 21, 2022, the patient tested positive for SARS-CoV-2, experiencing symptoms such as headaches, fever, fatigue, and myalgia. During the acute phase, the patient's highest body temperature was 38.7°C, and SPO2 was 96%. Notably, CSF and serum SARS-CoV-2 antibody tests showed positive results for IgG, indicating the potential influence of the virus on the central nervous system.
Therapeutic Interventions, Follow-Up, and Outcomes
A diagnosis of TDLs with multiple sclerosis prompted therapeutic interventions, including pulse therapy with methylprednisolone sodium succinate, gradually tapered to oral prednisone acetate. Follow-up imaging on May 2, 2023, revealed some improvement in TDLs but also the emergence of new lesions, prompting the recommendation for teriflunomide as disease-modifying treatment (DMT). However, two months into the DMT, imaging on July 9, 2023, indicated continued deterioration and the development of new lesions. Unfortunately, the patient refused further treatment and readmission, leaving the long-term course and effectiveness of teriflunomide in managing TDLs uncertain.
Discussion and Conclusion
This novel clinical case unveils a complex scenario where a patient with RRMS experiences the transformation into TDLs following a SARS-CoV-2 infection, challenging the efficacy of teriflunomide DMT. Several factors may contribute to this transformation, including the patient's pre-existing MS condition and the potential of SARS-CoV-2 to trigger relapses or transitions in MS. The virus's ability to induce a cytokine storm, disrupt the blood–brain barrier, and activate microglia and astrocytes may contribute to the worsening of MS symptoms and demyelination.
Moreover, the direct entry of SARS-CoV-2 into the brain through the olfactory pathway presents an additional layer of complexity. Studies have reported the presence of viral RNA in the brains of deceased COVID-19 patients, raising concerns about the direct neurotropic effects of the virus. The positive SARS-CoV-2 antibody results in the patient's CSF further support the notion of the virus's impact on the central nervous system.
This case serves as a poignant reminder of the challenges clinicians face in navigating the intricacies of MS diagnosis and treatment, especially in the context of a global pandemic. It underscores the need for comprehensive monitoring of MS patients, particularly in the post-SARS-CoV-2 infection period, with tailored interventions based on evolving clinical presentations.
The inefficacy of teriflunomide in controlling TDL transformation raises questions about the limitations of current disease-modifying therapies, urging the exploration of more targeted and effective medications for managing demyelinating diseases in the CNS. As we grapple with the uncertainties brought forth by the intersection of COVID-19 and neurological disorders, this case serves as a critical reference point for clinicians and researchers alike, emphasizing the necessity for further research and mechanistic studies to unravel the intricate interplay between SARS-CoV-2 and demyelinating diseases of the CNS. In forging ahead, collaborative efforts in the scientific community are paramount to gaining a comprehensive understanding of these complex interactions and improving patient outcomes in this uncharted territory.
The study findings were published in the peer reviewed journal: Frontiers in Neuroscience.
https://www.frontiersin.org/articles/10.3389/fnins.2023.1287480/full
For the latest
COVID-19 News, keep on logging to Thailand Medical News.