Polish Study Finds That Adenosine Deaminase 1 or ADA1 Hijacked by COVID-19 May be Fueling Long-Term Vascular Damage
Nikhil Prasad Fact checked by:Thailand Medical News Team May 21, 2025 8 months, 3 weeks, 2 days, 23 hours, 5 minutes ago
Medical News: COVID Virus Leaves Lasting Damage by Hijacking Natural Enzyme Pathways and Triggering Blood Vessel Inflammation
A groundbreaking new study has revealed that SARS-CoV-2, the virus responsible for COVID-19, may leave behind a lasting mark on the body by disrupting natural enzyme functions and triggering harmful inflammation in blood vessels, even after the infection is over. The research was led by scientists from the Department of Biochemistry, Department of Cardiac Diagnostics, and Laboratory of Tissue Engineering and Regenerative Medicine at the Medical University of Gdansk in Poland.
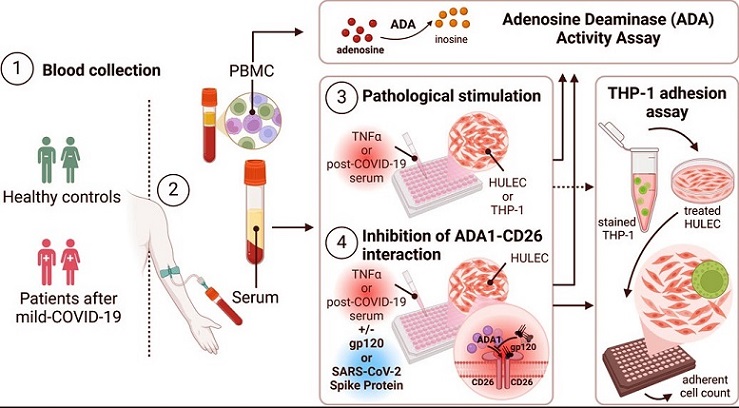
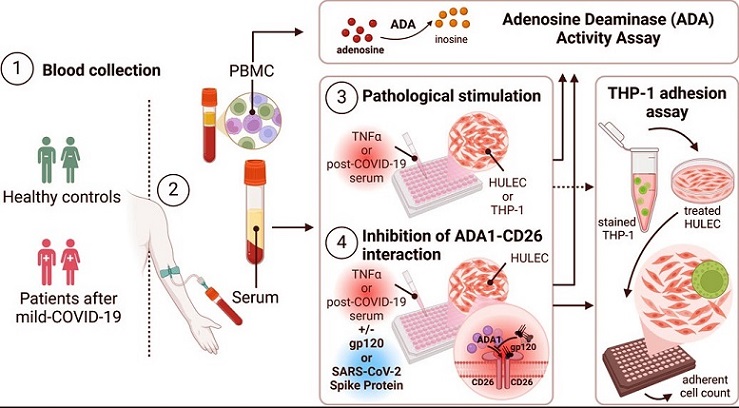 Graphical Abstract - Polish Study Finds That Adenosine Deaminase 1 or ADA1 Hijacked by COVID-19 May be Fueling Long-Term Vascular Damage
Graphical Abstract - Polish Study Finds That Adenosine Deaminase 1 or ADA1 Hijacked by COVID-19 May be Fueling Long-Term Vascular Damage
The study zeroes in on a key enzyme known as adenosine deaminase 1 (ADA1), which is normally involved in regulating inflammation and vascular health. Researchers discovered that after a COVID-19 infection, ADA1 becomes hyperactive and forms a damaging alliance with another molecule called CD26, creating a toxic cycle of inflammation in the lining of blood vessels. This
Medical News report will explore how this mechanism contributes to the long-haul symptoms experienced by many post-COVID patients.
The Dangerous Link Between ADA1 and CD26
In healthy individuals, ADA1 helps manage inflammation by breaking down adenosine, a molecule that acts as a natural anti-inflammatory agent. However, in post-COVID patients, the enzyme’s activity becomes excessive. The study showed that the blood of these patients contains high levels of ADA1 and CD26, especially in lung microvascular endothelial cells, the cells lining the interior of blood vessels in the lungs.
This unusual rise in ADA1 and CD26 leads to an increase in immune cell adhesion—essentially causing immune cells to stick more aggressively to blood vessel walls. This adhesive action contributes to prolonged inflammation and may explain why many people continue to suffer from symptoms like fatigue, chest pain, and shortness of breath long after their initial COVID-19 infection has resolved.
Unraveling the Mechanism with Real-World Samples
The researchers used blood samples from individuals who experienced lingering symptoms at least 12 weeks after a confirmed COVID-19 diagnosis. None of the participants had been vaccinated, allowing the team to study the virus’s effects without interference from vaccine-related immunity. When human lung endothelial cells were exposed to the serum from these post-COVID patients, there was a marked increase in both ADA1 and CD26 proteins, along with a rise in immune cell attachment.
What made these results more alarming was the discovery that blocking the interaction between ADA1 and CD26 using a molecule called glycoprotein 120 (gp120) significantly reduced this immune cell binding. This suggests that the ADA1-CD26 duo plays a central role in the ongoing inflammatory damage seen in post-COVID conditions.
SARS-CoV-2 Spik
e Protein Also Implicated
In an even more striking finding, the researchers observed that the spike protein of SARS-CoV-2—used by the virus to enter human cells—also attaches to CD26. When the spike protein was added to endothelial cells along with a pro-inflammatory agent (TNFα), it effectively mimicked the effects of the post-COVID serum, enhancing ADA1 activity and increasing inflammation.
However, when cells were treated with the spike protein beforehand, it blocked the rise in ADA1 activity typically induced by TNFα, suggesting a possible competitive binding mechanism. In other words, SARS-CoV-2 and ADA1 appear to be competing for the same docking site on CD26, and this competition may be influencing both the acute and long-term effects of the infection.
Implications for Post-COVID Complications
The study not only sheds light on how COVID-19 damages blood vessels during infection but also suggests why symptoms may persist for weeks or even months after recovery. By hijacking ADA1 pathways and altering its function, the virus seems to set off a cascade that primes the immune system for chronic inflammation. This may explain some of the cardiovascular issues, fatigue, and immune dysregulation seen in long COVID.
Importantly, the researchers propose that drugs which interfere with the ADA1-CD26 interaction—like sitagliptin, a diabetes medication that targets CD26—may hold promise for preventing or treating long-term COVID-related complications. Sitagliptin has already been linked to reduced mortality in hospitalized COVID patients, possibly due to its ability to block the same damaging pathways uncovered in this study.
Conclusion
This research provides critical insights into how SARS-CoV-2 continues to affect the body even after the virus is no longer detectable. By disrupting the balance of enzymes like ADA1 and hijacking cell-surface proteins such as CD26, the virus may be setting off a dangerous chain reaction that leads to chronic vascular inflammation and immune system dysfunction. The findings also open new doors for developing targeted therapies that can block this harmful interaction and help alleviate the long-term effects of COVID-19. With a growing number of people suffering from lingering symptoms, identifying and treating the root causes of post-COVID inflammation is now more important than ever.
The study findings were published in the peer reviewed journal: Frontiers in Pharmacology.
https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1578973/full
For the latest COVID-19 News, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/covid-19-can-trigger-deadly-autoimmune-hemolytic-anemia-which-often-shows-no-early-symptoms
https://www.thailandmedical.news/news/covid-19-news-weill-cornell-study-finds-that-sars-cov-2-infects-and-triggers-senescence-of-dopamine-neurons-metformin-helps
https://www.thailandmedical.news/news/covid-19-news-ukrainian-scientist-warns-that-the-alpha-7-nicotinic-acetylcholine-receptors-are-responsible-for-many-long-covid-manifestations
https://www.thailandmedical.news/articles/coronavirus
https://www.thailandmedical.news/pages/thailand_doctors_listings