Study Shows That SARS-CoV-2 Infections Causes Changes To The Fibrinolytic System With Hypofibrinolysis Common In Severe COVID-19
Thailand Medical News Team Aug 15, 2023 2 years, 6 months, 4 days, 16 hours, 23 minutes ago
COVID-19 News: The emergence of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in late 2019 brought about a global pandemic, challenging healthcare systems and causing a significant burden on societies worldwide. COVID-19, the disease caused by SARS-CoV-2, primarily affects the respiratory system but can also lead to systemic complications, including coagulopathy as covered in past studies, case reports and
COVID-19 News coverages. As researchers strive to decipher the intricate relationship between COVID-19 and the coagulation cascade, a recent study sheds light on how SARS-CoV-2 infection influences the fibrinolytic system and its implications for disease severity.
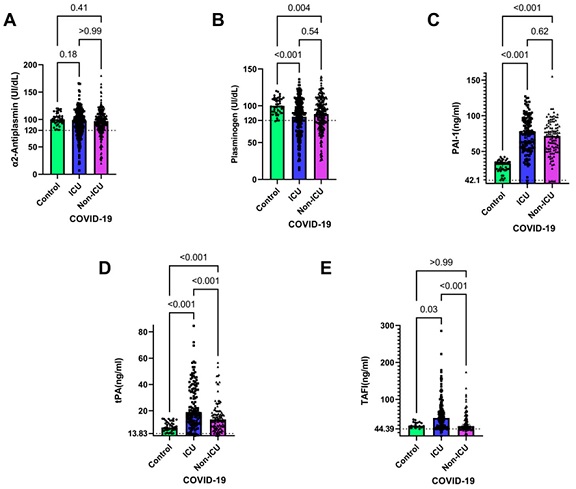
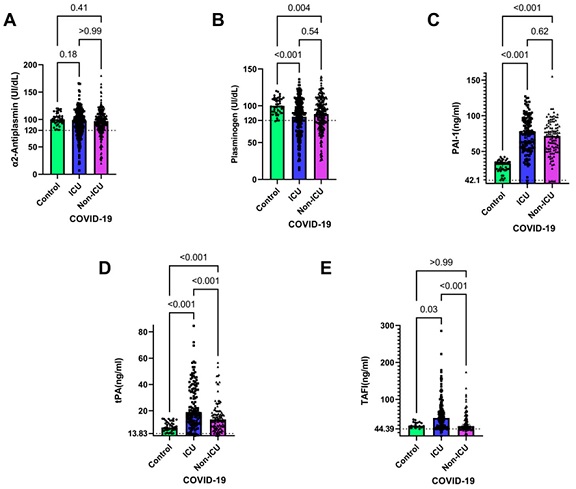 Coagulation parameters in ICU and non-ICU COVID-19 patients. Plasma isolated from blood samples of healthy individuals and COVID-19 patients either admitted or not admitted to the ICU were assessed for α2AP (A), plasminogen (B), PAI-1(C), tPA (D), and TAFI (E) were compared using the Kruskal–Wallis test. Levels of the aforementioned coagulation factors and p values are shown in each panel. The dotted lines represent the upper limit of the normal range for the plasma levels of all the coagulation markers. Data are represented as medians with 95% CI of n = 130 (ICU), n = 103 (non-ICU), n = 40 (healthy control)
The Fibrinolytic System - A Balancing Act
Coagulation parameters in ICU and non-ICU COVID-19 patients. Plasma isolated from blood samples of healthy individuals and COVID-19 patients either admitted or not admitted to the ICU were assessed for α2AP (A), plasminogen (B), PAI-1(C), tPA (D), and TAFI (E) were compared using the Kruskal–Wallis test. Levels of the aforementioned coagulation factors and p values are shown in each panel. The dotted lines represent the upper limit of the normal range for the plasma levels of all the coagulation markers. Data are represented as medians with 95% CI of n = 130 (ICU), n = 103 (non-ICU), n = 40 (healthy control)
The Fibrinolytic System - A Balancing Act
The fibrinolytic system is a complex physiological process that involves the breakdown of fibrin, the insoluble protein network that forms blood clots. In a healthy individual, this system maintains a delicate balance between pro-fibrinolytic factors that promote clot breakdown and anti-fibrinolytic factors that inhibit it. However, in various diseases, including respiratory conditions, cancer, and sepsis, this equilibrium can be disrupted, resulting in hypofibrinolysis (excessive clot formation) or hyperfibrinolysis (excessive clot breakdown).
Impact of COVID-19 on Fibrinolysis
Recent research conducted by scholars from esteemed Saudi Arabian institutions has delved into the intricate relationship between COVID-19 and the fibrinolytic system. This study investigated coagulation and fibrinolysis parameters in a cohort of 446 COVID-19 patients admitted between February 2021 and March 2022. The researchers aimed to understand how changes in the fibrinolytic system correlate with disease severity and outcomes.
Results and Findings
The study yielded significant insights into the impact of SARS-CoV-2 infection on the fibrinolytic system. Patients who succumbed to the disease exhibited markedly higher levels of thrombin activatable fibrinolysis inhibitor (TAFI), fibrinogen, and tissue plasminogen activator (tPA) compared to those who recovered. Notably, patients admitted to the intensive care unit (ICU) displayed elevated levels of plasminogen activator inhibitor-1 (PAI-1), tPA, and TAFI when compared to healthy controls.
Further analysis of disease stages revealed a noteworthy trend. Patients classified under stages C and D of COVID-19 severity exhibited significantly higher levels of PAI-1
, tPA, and TAFI. Moreover, patients in stage D demonstrated elevated tPA and TAFI values, reinforcing the association between disease progression and alterations in the fibrinolytic system.
Hypofibrinolysis: A Key Player in Severe COVID-19
One of the most significant observations from this study was the prevalence of hypofibrinolysis among patients with severe COVID-19. Hypofibrinolysis, characterized by reduced fibrinolytic activity and increased clot stability, was identified as a key factor in severe cases. Elevated levels of PAI-1 and TAFI were particularly pronounced in these patients, contributing to reduced fibrinolysis and a heightened risk of thrombotic events. Additionally, decreased levels of tPA, another important fibrinolytic factor, were reported in severe COVID-19 cases, further indicating impaired clot breakdown.
Unraveling the Mechanisms: How SARS-CoV-2 Impacts Fibrinolysis
The exact mechanisms by which SARS-CoV-2 influences the fibrinolytic system are still under investigation. However, several pathways have been proposed. The virus's activation of the immune system triggers an excessive release of pro-inflammatory cytokines, resulting in increased coagulation system activation. SARS-CoV-2 also directly infects cells involved in fibrinolysis regulation, such as blood platelets and blood vessel epithelial cells, exacerbating the activation of fibrinolysis. This hypercoagulable state contributes to thrombotic events and compromises the balance of the fibrinolytic system.
Clinical Implications and Future Directions
The findings of this study have important clinical implications for the management of COVID-19 patients. The identified coagulation markers, including PAI-1, tPA, and TAFI, hold promise as prognostic indicators for hypofibrinolysis and disease severity. Monitoring these markers in COVID-19 patients, particularly those with severe symptoms, could aid in predicting disease progression and guiding therapeutic interventions.
Furthermore, the study highlights the need for further research into the mechanistic underpinnings of the interaction between SARS-CoV-2 and the fibrinolytic system. Understanding these mechanisms at a molecular level could open avenues for the development of targeted therapeutic interventions to mitigate the impact of hypofibrinolysis and associated complications.
Conclusion
In conclusion, the study conducted by researchers from Saudi Arabian institutions underscores the significant alterations in the fibrinolytic system caused by SARS-CoV-2 infection. The prevalence of hypofibrinolysis among severe COVID-19 cases emphasizes the crucial role of the fibrinolytic system in disease progression. By identifying specific coagulation markers associated with disease severity, this study contributes to our understanding of COVID-19's complex pathophysiology and offers potential avenues for improved patient management. As the scientific community continues to unravel the intricate interplay between SARS-CoV-2 and the fibrinolytic system, these findings pave the way for more targeted and effective therapeutic strategies for COVID-19 patients.
The study findings were published in the peer reviewed Journal of Clinical Medicine.
https://www.mdpi.com/2077-0383/12/16/5223
For the latest
COVID-19 News, keep on logging to Thailand Medical News.