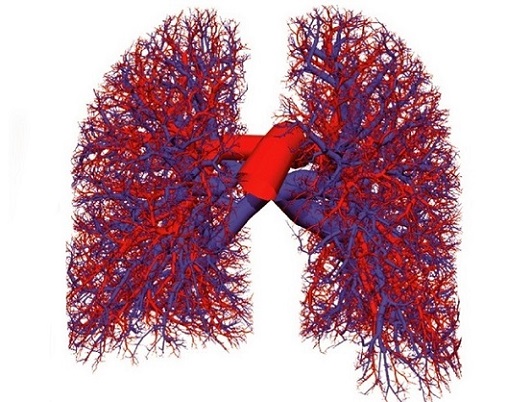
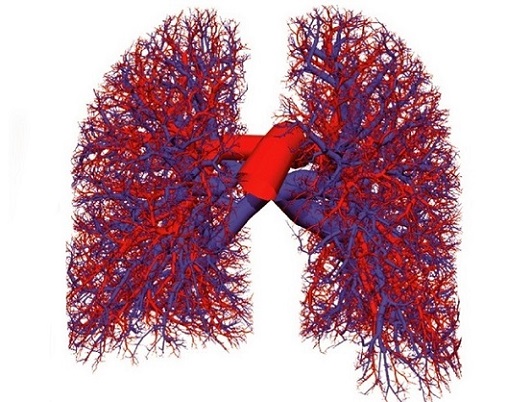
SARS-CoV-2 Spike Protein Causes Dangerous Remodeling of Lung Blood Vessels in the Dead and Likely in the Living as Well!
Nikhil Prasad Fact checked by:Thailand Medical News Team May 30, 2025 8 months, 3 weeks, 5 days, 2 hours, 18 minutes ago
Medical News: A new study by international researchers has revealed that severe COVID-19 is not just a respiratory illness but one that leaves lasting and possibly deadly damage to the lungs’ blood vessels. Scientists from Bogomolets National Medical University (Ukraine), Georgetown University (USA), Ivano-Frankivsk Regional Clinical Hospital (Ukraine), and the Medizinische Universität Lausitz-Carl Thiem (Germany) conducted a detailed investigation comparing lung tissues from deceased COVID-19 patients and those who died from H1N1 influenza.
 SARS-CoV-2 Spike Protein Causes Dangerous Remodeling of Lung Blood Vessels in the Dead and
SARS-CoV-2 Spike Protein Causes Dangerous Remodeling of Lung Blood Vessels in the Dead and
Likely in the Living as Well
The team analyzed 56 lung samples from people who died of COVID-19 and 17 samples from those who died during the 2009 H1N1 flu outbreak. Their goal was to study changes in the pulmonary arteries—major blood vessels in the lungs that are essential for oxygen exchange. This
Medical News report reveals the disturbing extent of damage caused by COVID-19, which far surpasses that caused by the flu.
COVID-19 Causes Severe Thickening and Scarring in Lung Blood Vessels
The researchers found that lung arteries in COVID-19 victims had significantly thickened walls. This was especially true in those who had been ill for more than 14 days. Unlike the flu group, the COVID-19 patients showed signs of what doctors call pulmonary vascular remodeling—a condition where blood vessel walls become abnormally thick and stiff. This was caused by several factors including hypertrophy (enlargement) of smooth muscle cells, buildup of fibrous tissue (perivascular fibrosis), inflammation, fluid retention, and even the formation of new blood vessels (neoangiogenesis) around the affected areas.
Using various stains and immunohistochemical techniques, the team confirmed that the virus’s spike protein had not only entered endothelial cells (cells lining blood vessels) but was also present in the smooth muscle cells. This suggests that the virus could directly damage these structures, rather than the damage being a secondary effect of inflammation.
Clear Link Between Disease Duration and Lung Vessel Damage
The study divided the COVID-19 cases into three groups based on how long the patient had been sick before dying: under 8 days, 9 to 13 days, and more than 14 days. The longer the disease lasted, the more severe the blood vessel thickening became. Measurements showed that in small arteries, the thickness of the muscular wall increased from 6.41 µm in early deaths to 13.49 µm in those sick for over two weeks. Similar increases were seen in medium-sized arteries. The area of the artery’s inner space (lumen), which carries blood, also shrank significantly, especially in longer infections.
Even more alarming, signs of arterial inflammation (vasculitis), blood clots (thrombosis), and iron buildup from bleeding (hemosiderosis) were common. In many patients, the blood vessels that feed other blood vessels&md
ash;called vasa vasorum—were clogged. This could create a cycle of worsening oxygen supply and tissue damage.
Spike Protein May Be Causing Direct Harm
What sets COVID-19 apart from flu, even severe H1N1, is its unique spike protein. This protein, which allows the virus to enter cells, binds to ACE2 receptors that are part of the body’s blood pressure system. By interfering with this system, the spike protein could be causing abnormal growth signals in vascular cells. It might even act directly to stimulate muscle and scar tissue buildup in the arteries.
The researchers also noted an unusually fast development of pulmonary hypertension—a dangerous condition where high blood pressure builds up in the lungs. This was confirmed by other studies using echocardiograms in COVID-19 patients, as well as multiple case reports from around the world. Some even suggested that the COVID-19 vaccines, which also use the spike protein, might trigger similar responses in rare cases.
Follow-Up for Survivors is Crucial
The study concludes that survivors of COVID-19, even those with mild symptoms, may not be out of danger. Pulmonary artery thickening and scarring were present even in those who did not show severe lung disease while alive. Therefore, the team stresses the need for long-term monitoring of COVID-19 patients for signs of pulmonary hypertension and vascular complications.
In conclusion, the research highlights that SARS-CoV-2 is not just a respiratory virus but one that deeply affects the vascular system, especially the arteries in the lungs. This damage is more severe and distinct from that seen in H1N1 influenza. It involves multiple mechanisms including direct infection of muscle cells in arteries, fibrosis, new vessel formation, inflammation, and oxygen starvation due to thrombosis. These findings raise serious concerns about the long-term health of COVID-19 survivors and the hidden burden of vascular disease that may emerge in the years ahead.
The study findings were published in the peer-reviewed journal: COVID (MDPI).
https://www.mdpi.com/2673-8112/5/6/79
For the latest COVID-19 News, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/covid-19-damages-human-blood-vessels
https://www.thailandmedical.news/news/sars-cov-2-suppresses-membrane-complement-regulatory-proteins-making-blood-vessels-more-vulnerable-to-damage-
https://www.thailandmedical.news/news/polish-study-finds-that-adenosine-deaminase-1-or-ada1-hijacked-by-covid-19-may-be-fueling-long-term-vascular-damage
https://www.thailandmedical.news/articles/coronavirus
https://www.thailandmedical.news/pages/thailand_doctors_listings