Kittisak Meepoon Fact checked by:Thailand Medical News Team Dec 04, 2025 3 months, 2 days, 13 hours, 47 minutes ago
Medical News: Study Finds Lasting Brain Changes in COVID-19 Survivors Affecting Emotion and Memory
A new groundbreaking study has revealed that COVID-19 can cause long-term damage to specific brain regions, especially the basal ganglia and limbic system. These areas are crucial for controlling memory, emotion, behavior, and movement. Even months after recovery, many COVID-19 survivors continue to show changes in these critical parts of the brain, raising serious concerns about the long-term neurological impact of the virus.
 COVID-19 causes long-term structural brain damage in regions controlling memory and emotion, even after recovery
COVID-19 causes long-term structural brain damage in regions controlling memory and emotion, even after recovery
The research was led by teams from the Indian Institute of Technology Delhi, New York University Abu Dhabi, and the New Jersey Institute of Technology. Using advanced multimodal MRI scans, they examined the brains of 76 people who had recovered from COVID-19 and compared them with 51 healthy individuals. This
Medical News report brings attention to how even non-hospitalized COVID-19 patients can suffer from hidden brain injuries.
No Total Brain Shrinkage but Key Regions Affected
The study found no difference in overall brain volume between COVID-19 survivors and healthy controls. However, MRI scans revealed that specific brain regions—particularly in the right hemisphere—had reduced size in those who had previously been infected. These included the thalamus, hippocampus, amygdala, putamen, caudate, and pallidum—all of which are part of the basal ganglia and limbic system.
Researchers also observed thinning and reduced volume in parts of the brain’s cortex, especially the insular cortex and superior temporal gyrus. These areas are involved in emotional regulation, social behavior, and attention—symptoms that many long COVID sufferers still report.
White Matter Damage and Severe Cases Show More Change
The study also revealed changes in the brain’s white matter—the part responsible for connecting different brain regions. Damage was especially seen in tracts related to the limbic system, such as the uncinate fasciculus and cingulum. These changes were more severe in patients who had been hospitalized, suggesting that the more intense the infection, the more significant the brain alterations.
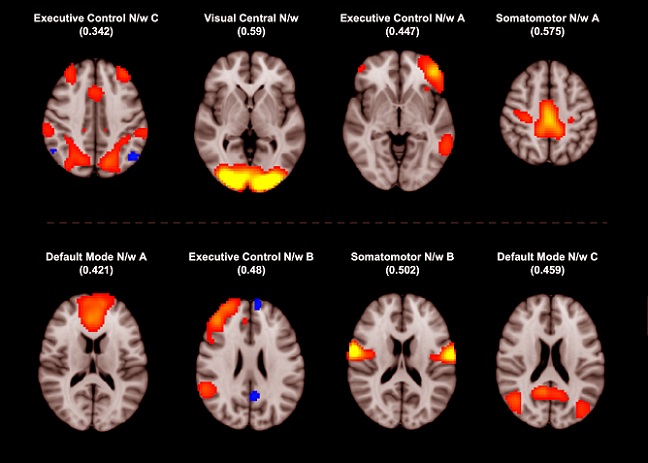
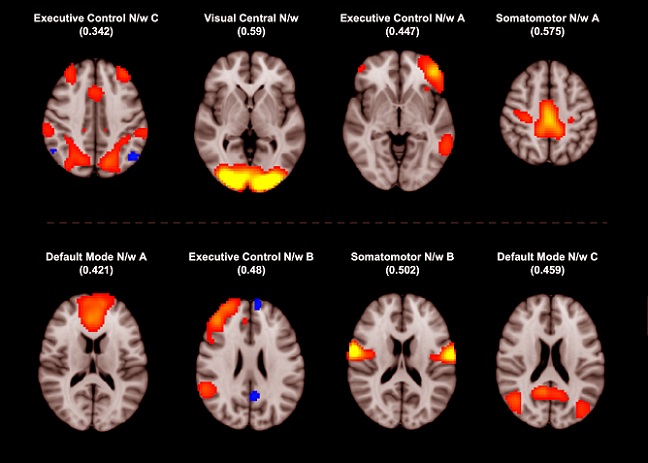
In hospitalized patients, functional MRI scans showed reduced connectivity in important brain networks, including the default mode network and connections with the caudate and insula. These disruptions are believed to contribute to ongoing issues like fatigue, sleep problems, brain fog, and emotional instability.
No Clear Blood Flow Reductions Found
Unlike some earlier studies, this research did not detect any major differences in brain blood flow between COVID-19 survivors and healthy individuals, suggesting that the structural and functional changes are not due to reduced blood supply but possibly from inflammation or immune responses during infection.
These fi
ndings offer critical insight into how COVID-19 can silently affect the brain long after recovery. They highlight the urgent need for continued monitoring and support for survivors, even those who had only mild or moderate symptoms.
The study findings were published in the peer reviewed journal: Imaging Neuroscience
https://direct.mit.edu/imag/article/doi/10.1162/IMAG.a.1027/133912/Multimodal-MRI-reveals-consistent-basal-ganglia
For the latest COVID-19 news, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/articles/coronavirus
https://www.thailandmedical.news/articles/long-covid