COVID-19 News -Bipolar Disorder Mar 10, 2023 2 years, 11 months, 1 week, 6 days, 16 hours, 52 minutes ago
COVID-19 News: The world has been facing the COVID-19 pandemic for the past 3 years. With over 3 billion people already possibly exposed to the SARS-CoV-2 virus and more than 47 million deaths worldwide including excess deaths, the ongoing COVID-19 pandemic has posed one of the biggest challenges to modern medicine.

The COVID-19 pandemic has caused not only physical health problems but also social and economic consequences. One of the significant health consequences of COVID-19 is the development of neuropsychiatric diseases, such as anxiety and depression along with a wide range of mental disorders.
Reports of (hypo)manic episodes and bipolar disorder after experiencing COVID-19 are starting to emerge in scientific literature and in various
COVID-19 News coverages.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9453104/
https://www.mdpi.com/2077-0383/11/20/6060#B24-jcm-11-06060
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9240303/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7722969/
https://www.thailandmedical.news/news/breaking-covid-19-news-italian-researchers-warn-that-sars-cov-2-infections-can-lead-to-new-onset-psychosis-expect-more-loonies-walking-around
https://europepmc.org/article/med/34904342
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8652648/
https://www.sciencedirect.com/science/article/pii/S0165032720326276
https://casereports.bmj.com/content/13/6/e236123.abstract
https://www.sciencedirect.com/science/article/pii/S0967586821000850
https://www.qscience.com/content/journals/10.5339/qmj.2021.65
Mania is an integral part of bipolar disorder (BD), a debilitating illness. Therefore, it is essential to determine whether SARS-CoV-2 infection is a causative agent of this severe mental disorder.
Psychiatric disorders, such as major depressive disorder (MDD), generalized anxiety disorders (GAD), post-traumatic
stress disorder (PTSD), obsessive-compulsive disorder (OCD), sleep disorders, and cognitive and memory disorders, are frequently described in connection with COVID-19.
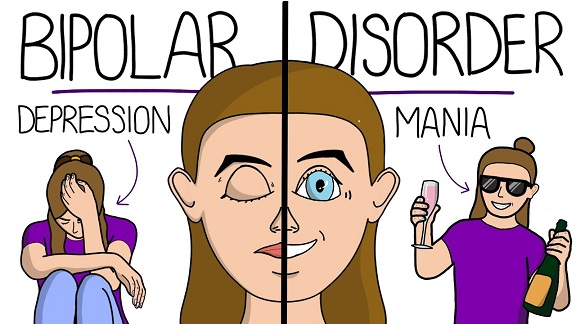
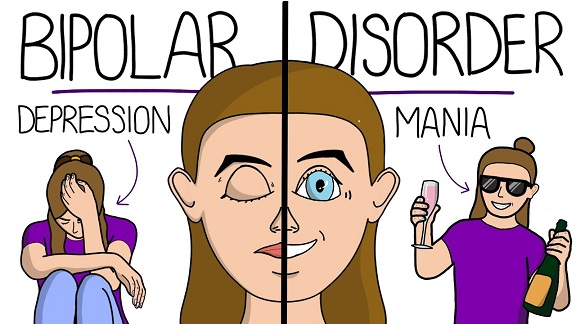
Bipolar Disorder or BD is a type of affective disorder characterized by recurring episodes of depression and mania or hypomania with possible psychotic symptoms. It most often begins in young people and affects men and women equally.
Bipolar Disorder is a neuroprogressive disorder, meaning that there is a gradual clinical and functional deterioration of the patient's condition. Changes in neuroplasticity, deficiencies in neurotrophic factors, oxidative stress, inflammation, and circadian rhythm disturbances are associated with exacerbation of affective episodes, treatment resistance, and cognitive and functional dysfunctions.
As BD is a neuroprogressive disorder, detecting it at the earliest possible stage or being prepared for the possibility of its development is critical. This would allow for the quick implementation of appropriate treatment to minimize the effects of the disease and maximize patients' years of life with a quality similar to that of healthy people.
It has a significant impact on the quality of life and its mental and physical zones. The lifetime prevalence of Bipolar Disorder or BD ranges from 0.1% to 2.4%. The key elements of BD are manic or hypomanic episodes, which are characterized by increased mood, hyperactivity, impulsiveness, grandiosity, increased self-esteem, decreased anxiety, decreased need for sleep, increased sex drive, and in some cases psychosis.
The etiopathogenesis of bipolar disorder is still largely unknown, although there are many hypotheses that take into account factors such as inflammation and its markers, changes in genetics and epigenetics, metabolism, hormones, neurotransmission and immunology as well as oxidative stress and external stressors.
Past analysis of 22 publications that describe 36 patients who experienced a manic or hypomanic episode correlated with COVID-19 and a further analysis of 108 publications regarding biomarkers and frequent changes in bipolar disorder patients and 70 publications regarding disorders connected to SARS-CoV-2 infection and compared them to identify the possible causes of hypo(mania) and potential bipolar disorder or BD in COVID-19 patients have revealed interesting findings.
https://www.mdpi.com/2077-0383/11/20/6060#B24-jcm-11-06060
It was found that the majority of the patients who experienced a manic or hypomanic episode correlated with COVID-19 were male, of different ages and nationalities, and had no family history of mental disorders. The severity of COVID-19 was different among them, and manic symptoms developed at varying time intervals from the onset of COVID-19 symptoms. The most common symptoms of mania among them were insomnia, elevated mood, agitation, irritability, delusions, grandiosity, and talkativeness.
The researchers in the above study collected previously reported cases of (hypo)mania that occurred in patients after infection with the SARS-CoV-2 virus, both in those who had never been treated for psychiatric diseases and in those with a psychiatric history. These descriptions are in many cases inconsistent, differ in the manner of examination and diagnostics, and access to all data is impossible. Therefore, it is difficult to talk about a reliable analysis of all the factors that could have caused a manic episode in the patients they collected. Nevertheless, they decided that the mere appearance of them shortly after infection with SARS-CoV-2 is a sufficient reason to analyze the similarities between the disorders caused by the infection and those that are present in patients with bipolar disorder or BD in order to assess whether SARS-CoV-2 may be a risk factor for developing this disorder.
The researchers divided the disorders of homeostasis that occur in patients with bipolar disorder or BD and its recognized risk factors into nine categories: (a) cytokine and inflammatory disorders, (b) use of corticosteroids, (c) HPA axis disorders, (d) sleep disorders, (e) BDNF deficiency, (f) hyperactivity of the kynurenine pathway, (g) structural changes in the CNS, (h) neurotransmission disorders, and (i) oxidative stress. These factors create a complex system in which most of them interact with each other, creating a self-reinforcing cycle that results in the development of affective disorders, including bipolar disorders or BD.
The study findings showed that SARS-CoV-2 infection affects most of the above-mentioned factors with varying severity. In their opinion, the most visible disorder that occurs in SARS-CoV-2 and that may affect the development of bipolar disorder or BD in patients is systemic inflammation and cytokine storm.
Another clearly visible disorder in COVID-19 is the activation of the kynurenine pathway through increased activation of IDO under cytokine storm conditions which can also lead to bipolar disorders.
Yet, another disorder that has a strong similarity between SARS-CoV-2 and bipolar disorder or BD patients is oxidative stress. Brain disorders in patients with SARS-CoV-2 similar to those in patients with BD and which may influence the development of its symptoms are mainly white matter abnormalities. The above-mentioned inflammatory cytokines, kynurenine metabolites, and oxidative stress contribute to the development of white matter anomalies and disorders of nerve signal transduction. Another common point of bipolar disorder or BD and SARS-CoV-2 is sleep disturbance.
An additional risk factor if for is corticosteroid therapy during hospitalization of infected patients.
In conclusion, the disorders caused by SARS-CoV-2 overlap with those found in bipolar disorder or BD patients, and COVID-19, especially with severe course, may be a risk factor for the development of BD in particularly vulnerable people, e.g., with a family history, or lead to relapse in previously diagnosed BD patients.
Clinicians should be aware of the possibility of developing affective episodes, including mania, in vulnerable patients and extend the follow-up period after discharge from the hospital as some post-COVID depression may turn out to be misdiagnosed BD over time.
For the latest
COVID-19 News, keep on logging to Thailand Medical News.