Nikhil Prasad Fact checked by:Thailand Medical News Team Oct 01, 2024 1 year, 4 months, 2 weeks, 4 days, 4 hours, 32 minutes ago
Medical News: The global COVID-19 pandemic has significantly impacted the health of millions worldwide. While most cases of COVID-19 result in mild symptoms, a smaller but critical proportion of patients experience severe illness, often requiring intensive care. A recent study conducted by researchers from Guangzhou Medical University and affiliated institutions in China provides insight into the immune dysfunction observed in patients with severe COVID-19. This
Medical News report explores key findings of the study, aiming to explain complex medical concepts in a simple and clear manner.
 T Cell Dysfunction and Immune Suppression in Severe COVID-19 Patients
Study Overview
T Cell Dysfunction and Immune Suppression in Severe COVID-19 Patients
Study Overview
The researchers used advanced single-cell RNA sequencing (scRNA-seq) technology to analyze immune cells from severe COVID-19 patients, focusing on the pleural fluid and blood samples. The analysis identified significant immune dysregulation, particularly involving T cell exhaustion and macrophage polarization, which may play a role in the severity of the disease.
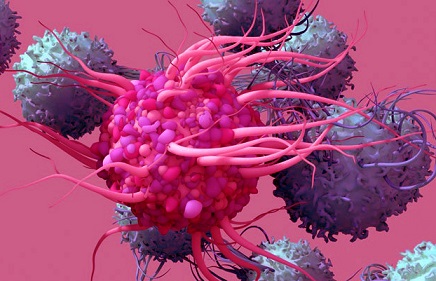
T Cell Dysfunction and Exhaustion
The study revealed that T cells, which are crucial for fighting off infections, become hyperactivated and eventually exhausted in severe COVID-19 patients. T cells are a type of white blood cell that plays a vital role in the immune response by identifying and destroying infected cells. However, when these cells are overworked due to persistent viral infection, they lose their effectiveness.
The researchers observed this T cell exhaustion predominantly in the pleural fluid, which surrounds the lungs, rather than in the blood. This discovery suggests that the local immune environment in the lungs plays a crucial role in disease progression. The presence of hyperactivated and exhausted T cells in the lungs could delay viral clearance and contribute to the severity of respiratory symptoms.
Role of Macrophages in Immune Suppression
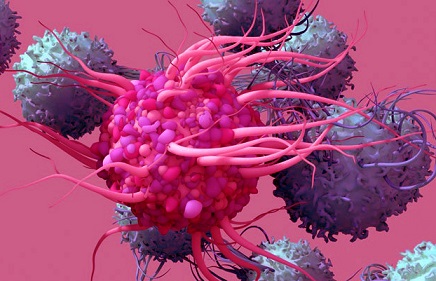
Another important finding was the role of macrophages in driving immune suppression. Macrophages are immune cells responsible for engulfing and digesting pathogens, such as bacteria and viruses. In severe COVID-19 cases, the researchers found that a particular type of macrophage, known as M2 macrophages, was highly prevalent in the pleural fluid of patients.
M2 macrophages are typically involved in wound healing and tissue repair, but in this context, they were found to produce anti-inflammatory signals that suppress T cell activity. These macrophages secrete molecules like IL-10, which dampen the immune response and contribute to T cell exhaustion. The study suggests that M2 macrophage polarization may create an immunosuppressive environment in the lungs, making it harder for the body to fight off the virus effectively.
Transposable Elements and Their Role in COVID-19
The study also explored the expression of transposable elements (TEs) in severe COVID-19 patients. Transposable elements are segments of DNA that can change their position within the genome, and
they play a role in regulating immune responses. The researchers found that TEs were differentially expressed in severe COVID-19 patients compared to those with mild cases.
Notably, TEs were upregulated in monocytes and macrophages, the very cells involved in immune suppression. This suggests that the regulation of these genetic elements may contribute to the immune dysfunction seen in severe COVID-19 cases. Although the exact role of TEs in the disease is still being investigated, their involvement highlights the complexity of the immune response to SARS-CoV-2, the virus that causes COVID-19.
The Importance of Pleural Fluid Analysis
One of the key takeaways from the study is the importance of analyzing pleural fluid in severe COVID-19 cases. While blood samples provide valuable information about the overall immune response, the pleural fluid more accurately reflects the local immune environment in the lungs, where the virus causes the most damage. The researchers emphasize that pleural fluid analysis offers a more reliable indicator of immune dysregulation in severe COVID-19 patients, particularly when it comes to T cell function and macrophage activity.
Therapeutic Implications
Understanding the mechanisms behind immune dysfunction in severe COVID-19 patients opens up potential avenues for treatment. The study's findings suggest that targeting M2 macrophages or the molecules they produce, such as IL-10, could help restore T cell function and improve patient outcomes. Some existing cancer therapies that target M2 macrophages or enhance the activity of other immune cells could be repurposed for COVID-19 treatment.
Additionally, therapies that stimulate T cell activity, such as thymosin (Zadaxin), have shown promise in improving immune function in COVID-19 patients. The study observed that patients treated with Zadaxin experienced an increase in the number of natural killer (NK) cells and CD8+ T cells, which are important for controlling viral infections.
Study Limitations and Future Research
While the study provides valuable insights into the immune dysregulation seen in severe COVID-19 patients, it also has limitations. The analysis was based on a small sample size, and not all COVID-19 patients develop pleural effusion, the excess fluid around the lungs that was analyzed in this study. Therefore, future research should aim to include a larger and more diverse patient population to validate these findings.
Moreover, the exact role of transposable elements in COVID-19 remains unclear, and further studies are needed to explore how these genetic elements contribute to the disease process. Understanding the interplay between TEs, macrophages, and T cells could lead to new therapeutic strategies for treating severe COVID-19 cases.
Conclusion
This study sheds light on the complex immune dysfunction that occurs in severe COVID-19 patients, particularly the role of T cell exhaustion and macrophage-driven immune suppression. The findings highlight the importance of local immune environments, such as the pleural fluid, in understanding disease severity and suggest potential therapeutic targets for improving patient outcomes. As research into COVID-19 continues, these insights will be crucial for developing more effective treatments for those at highest risk of severe illness.
The study findings were published in the peer-reviewed journal: Heliyon.
https://www.sciencedirect.com/science/article/pii/S2405844024147196
For the latest COVID-19 News, keep on logging on to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/sars-cov-2-e-protein-induces-long-term-immune-dysfunction
https://www.thailandmedical.news/news/canadian-study-find-that-persistent-immune-dysfunction-as-being-behind-lethality-in-both-covid-19-and-non-covid-19-sepsis