Nikhil Prasad Fact checked by:Thailand Medical News Team May 27, 2024 1 year, 8 months, 2 weeks, 6 days, 4 hours, 44 minutes ago
Medical News: The pancreas, a remarkable organ performing both exocrine and endocrine functions, plays a vital role in our body's metabolic homeostasis. It produces digestive enzymes through acinar cells and vital hormones such as insulin and glucagon via the islet cells of Langerhans. The pancreas' microenvironment, composed of a myriad of cells including endothelial, ductal, neural, and immune cells, relies on intricate cellular crosstalk to maintain its structural and functional integrity. However, disruptions in this communication can lead to severe pancreatic diseases like pancreatitis, diabetes, and pancreatic cancer.
 Macrophages - Key Players in Pancreatic Diseases
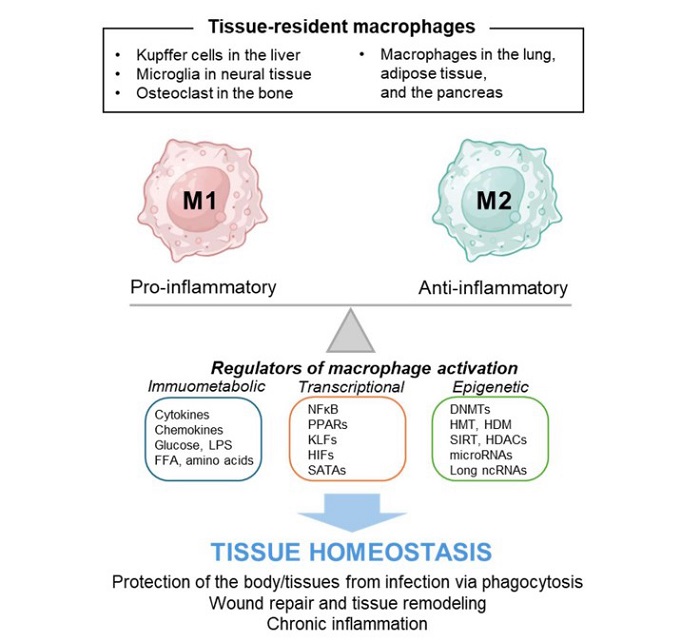
Schematic diagram of macrophage polarization and its regulators. Macrophages respond to changes in the tissue microenvironment by altering their polarity towards M1 or M2, thus playing a role in regulating tissue homeostasis. They engage in phagocytosis to combat infections and contribute to tissue remodeling through wound repair. Additionally, macrophages can induce chronic inflammation, which disrupts the tissue microenvironment. Abnormal macrophage polarization can contribute to the development of pancreatitis, diabetes, and cancer. Various immunometabolic, transcriptional, and epigenetic factors influence macrophage polarization towards M1 or M2 phenotypes, and identifying new regulators is essential for understanding macrophage-mediated tissue homeostasis.
Macrophages - Key Players in Pancreatic Diseases
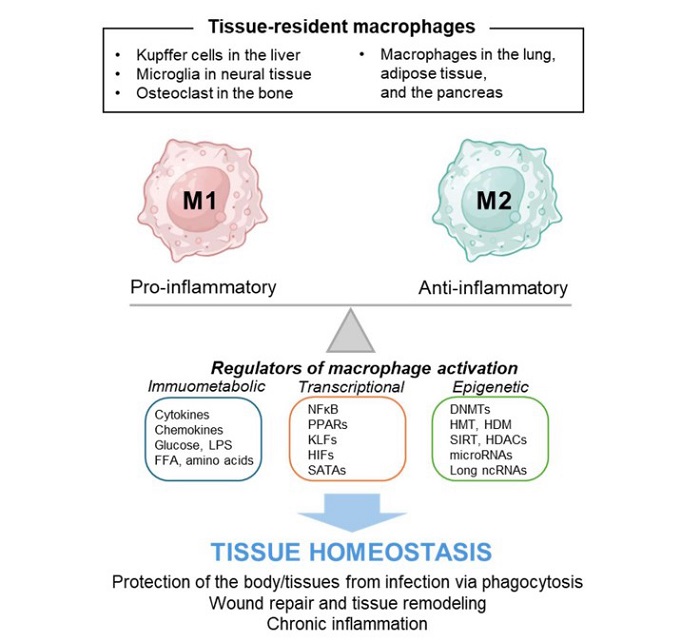
Schematic diagram of macrophage polarization and its regulators. Macrophages respond to changes in the tissue microenvironment by altering their polarity towards M1 or M2, thus playing a role in regulating tissue homeostasis. They engage in phagocytosis to combat infections and contribute to tissue remodeling through wound repair. Additionally, macrophages can induce chronic inflammation, which disrupts the tissue microenvironment. Abnormal macrophage polarization can contribute to the development of pancreatitis, diabetes, and cancer. Various immunometabolic, transcriptional, and epigenetic factors influence macrophage polarization towards M1 or M2 phenotypes, and identifying new regulators is essential for understanding macrophage-mediated tissue homeostasis.
The
Medical News report cover a study review by researchers from The Catholic University of Korea, Seoul-Republic of Korea on how macrophages can be either ‘villains’ or ‘heroes’ in various pancreatic diseases.
Macrophages: The Immune Gatekeepers
Macrophages, the dynamic immune cells, are central to the immune responses in the pancreas. Originating from monocytes in the bone marrow, these cells migrate to various tissues where they differentiate based on the local microenvironment. Their role extends beyond phagocytosis; they also secrete cytokines, chemokines, and growth factors that regulate inflammation, tissue repair, and immune responses.
Macrophages exhibit remarkable plasticity, toggling between pro-inflammatory (M1) and anti-inflammatory (M2) states. This ability to shift between M1 and M2 states makes macrophages critical in maintaining pancreatic homeostasis. Their dysfunction, however, can drive the pathogenesis of pancreatic diseases.
Macrophages in Pancreatitis
Pancreatitis, characterized by inflammation of the pancreas, can manifest as either acute (AP) or chronic (CP). Various triggers such as gallstones, alcohol, smoking, hyperglycemia, and genetic mutations can initiate pancreatitis. In acute pancreatitis, macrophages play a crucial role by releasing pro-inflammatory cytokines that exacerbate the condition. Persistent inflammation leads to chronic pancreatitis, marked by fibrosis and an increased risk of pancreatic cancer.
<
;br />
Acute Pancreatitis: The Initial Assault
During AP, pancreatic injury leads to the activation of macrophages, which release inflammatory cytokines like TNF-α, IL-1β, and IL-6, amplifying the inflammatory response. The role of macrophages in this initial phase is dual-faceted; while they attempt to resolve inflammation, their overactivation can worsen the condition. Factors like the mixed-lineage kinase domain-like protein (MLKL) and microRNAs such as miR-29a significantly influence macrophage polarization and, consequently, the severity of AP.
Chronic Pancreatitis: The Prolonged Battle
In CP, continuous pancreatic injury results in excessive extracellular matrix production, leading to fibrosis. Macrophages in CP often adopt an M2 phenotype, which, while anti-inflammatory, promotes fibrosis and disease progression. Cytokines like IL-4 and IL-13, primarily from pancreatic stellate cells (PSCs), drive this M2 polarization. The intricate interplay between macrophages and other cellular components highlights the complexity of CP pathogenesis and the potential for targeted therapies that modulate macrophage activity.
Macrophages in Diabetes
Diabetes, a systemic disease characterized by insulin deficiency or resistance, affects multiple organs, including the pancreas. Macrophages play a pivotal role in maintaining tissue homeostasis within the islets of Langerhans, where they interact with β cells and other cellular components. Dysregulation in this crosstalk can lead to β cell dysfunction and exacerbate diabetes.
Islet Dysfunction and Immune Interaction
Islet dysfunction is a primary driver of insulin resistance. Macrophages within the islets, influenced by factors secreted by β cells, can either protect or damage the islet microenvironment. For instance, pancreatic β cells secrete molecules like CSF1 and IL-1β, which modulate macrophage activity. Therapeutic strategies aiming to alter macrophage polarization, such as co-culturing with mesenchymal stem cells or glucagon-like peptide-1 treatment, have shown promise in protecting β cells and improving diabetes outcomes.
Peripheral Tissues and Systemic Impact
Beyond the pancreas, macrophages in peripheral tissues like the kidneys and adipose tissues also play critical roles in diabetes. Factors like hyperoside and miRNAs have been shown to influence macrophage polarization, thereby impacting insulin resistance and diabetic complications. Understanding these interactions offers potential therapeutic avenues to manage diabetes and its systemic effects.
Macrophages in Pancreatic Cancer
Pancreatic ductal adenocarcinoma (PDAC), the most common form of pancreatic cancer, is characterized by a complex tumor microenvironment (TME). Macrophages, particularly M2-polarized tumor-associated macrophages (TAMs), are pivotal in PDAC progression. These cells support tumor growth and metastasis by creating an immunosuppressive environment, which hinders effective immune responses and treatment efficacy.
The Tumor Microenvironment
The TME of PDAC is enriched with M2 macrophages, which facilitate tumor progression through various mechanisms. Proteins like IGFBP2 and PKM2, upregulated in PDAC tissues, promote M2 polarization and enhance tumor growth. Strategies targeting these proteins, as well as interventions aiming to reprogram TAMs, are being explored to improve PDAC treatment outcomes.
Discussion and Future Directions
The pivotal role of macrophages in pancreatic diseases underscores the importance of understanding their regulatory mechanisms. Future research should focus on elucidating the detailed pathways that control macrophage polarization and their interactions with other cellular components. Advanced technologies like single-cell RNA sequencing and proteomics can provide deeper insights into the cellular heterogeneity of the pancreas and identify new therapeutic targets.
Moreover, the role of microbiota in regulating pancreatic microenvironment highlights an additional layer of complexity. Understanding microbiota-mediated crosstalk and its impact on macrophage behavior could pave the way for novel therapeutic strategies.
Conclusion
Macrophages, with their ability to switch between pro-inflammatory and anti-inflammatory states, are central to the pathophysiology of pancreatitis, diabetes, and pancreatic cancer. Understanding the factors that regulate macrophage polarization is crucial for developing targeted therapies that can modulate inflammatory and fibrotic responses in pancreatic diseases. Advances in this field hold the promise of improving patient outcomes and paving the way for effective management and potential cures for these challenging conditions.
The study findings were published in the peer reviewed International Journal of Molecular Sciences.
https://www.mdpi.com/1422-0067/25/11/5765
For the latest about Pancreatic Diseases, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/breaking-covid-19-latest-sars-cov-2-induces-immunoparalysis-of-human-host,-infects-monocytes,-macrophages-and-can-cause-fibrosis-in-post-covid-19
https://www.thailandmedical.news/news/new-immunotherapy-target-identified-in-treating-pancreatic-cancer.
https://www.thailandmedical.news/news/coronavirus-news-cedars-sinai-medical-center-study-confirms-that-the-sars-cov-2-virus-infects-the-pancreas-directly