Australian Study Uncovers Roles Of The Kynurenine Pathway In COVID-19 Neuropathogenesis
Nikhil Prasad Fact checked by:Thailand Medical News Team May 29, 2024 1 year, 8 months, 2 weeks, 3 days, 22 hours ago
COVID-19 News: In the early days of the COVID-19 pandemic, much of the focus was on the respiratory symptoms and the acute phase of the disease. However, as the pandemic progressed, it became clear that COVID-19 is not just a respiratory illness but a multi-system disease that can have lasting effects, particularly on the neurological system. Researchers from Macquarie University in Sydney, the University of Melbourne at the Peter Doherty Institute for Infection and Immunity, and St. Vincent’s Centre for Applied Medical Research in Sydney have delved into the complex interactions between SARS-CoV-2 and the kynurenine pathway (KP), uncovering significant insights into how this pathway may contribute to COVID-19's neurological impacts. These findings are covered in this exclusive
COVID-19 News report.
 The roles of the kynurenine pathway in COVID-19 neuropathogenesis
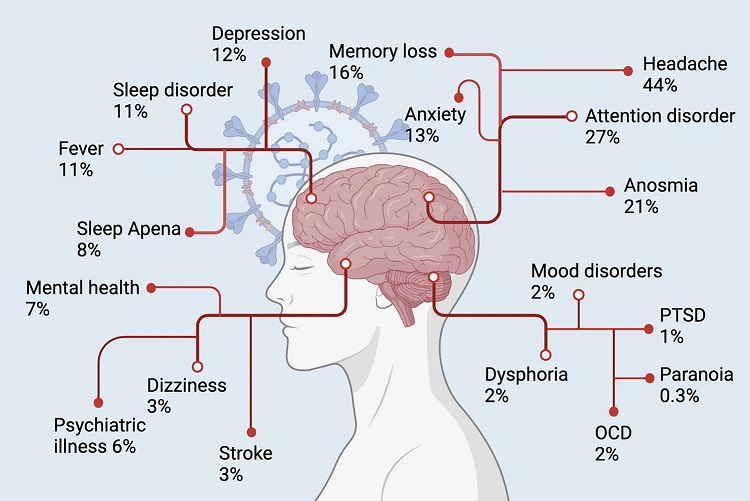
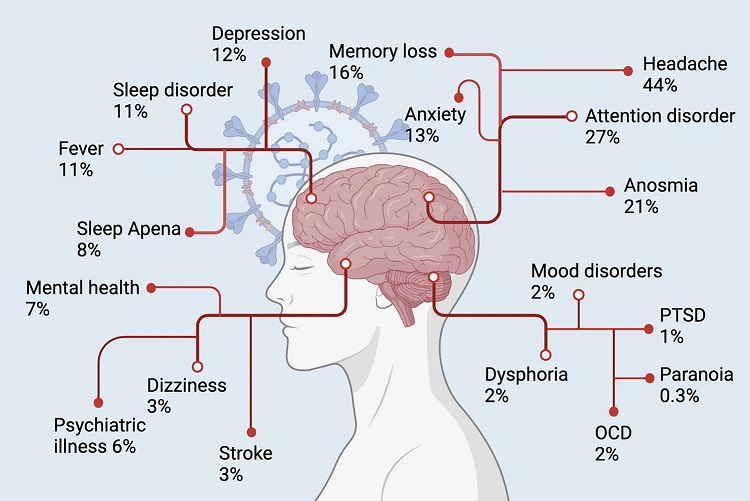
Neuropsychiatric symptoms associated with long-COVID-19. The prevalence of neuropsychiatric symptoms was estimated according to a meta-analysis performed with 15 different peer-reviewed studies including 47,910 patients (age 17–87 years).
The Kynurenine Pathway: An Overview
The roles of the kynurenine pathway in COVID-19 neuropathogenesis
Neuropsychiatric symptoms associated with long-COVID-19. The prevalence of neuropsychiatric symptoms was estimated according to a meta-analysis performed with 15 different peer-reviewed studies including 47,910 patients (age 17–87 years).
The Kynurenine Pathway: An Overview
L-tryptophan (Trp) is an essential amino acid involved in several metabolic processes, including the kynurenine pathway (KP) and the serotonin pathway. Approximately 95% of Trp is metabolized through the KP, leading to the production of various neuroactive metabolites such as kynurenine (KYN), kynurenic acid (KYNA), 3-hydroxykynurenine (3-HK), and quinolinic acid (QUIN). These metabolites play crucial roles in both neurological and immune functions. For instance, KYNA is known for its neuroprotective properties, whereas QUIN is recognized as a neurotoxin that can contribute to neurodegeneration.
The enzyme indoleamine 2,3-dioxygenase 1 (IDO-1) catalyzes the first step of the KP, converting Trp into KYN. This enzyme is particularly interesting in the context of COVID-19 because its activity can be significantly increased by pro-inflammatory cytokines such as interferon-gamma (IFN-γ), interleukin-6 (IL-6), and tumor necrosis factor-alpha (TNF-α). These cytokines are typically elevated during the acute phase of COVID-19, especially in severe cases where a cytokine storm occurs.
SARS-CoV-2 and the Kynurenine Pathway
SARS-CoV-2, the virus responsible for COVID-19, has been shown to affect various metabolic pathways in infected individuals. Studies have reported significant increases in the levels of KP metabolites such as QUIN and 3-HK in patients with COVID-19. These metabolites are not only neurotoxic but also contribute to the modulation of the immune system, suggesting that the KP might play a critical role in the pathogenesis of COVID-19, particularly in its neurological manifestations.
The study utilizing untargeted metabolomics analyses has revealed that Trp metabolism is one of the most significantly modulated pathways in SARS-Co
V-2-infected individuals. Marked decreases in Trp and serotonin levels, alongside increases in KYN, picolinic acid (PIC), and KYNA, highlight the activation of the KP in COVID-19 patients. This activation is especially prominent in patients experiencing cognitive impairment as part of the post-acute sequelae of COVID-19 (PASC), also known as long COVID.
Mechanisms Behind KP Activation in COVID-19
The exact mechanisms by which COVID-19 triggers changes in the KP are complex and multifaceted. The cytokine storm observed in severe cases of COVID-19 leads to the activation of IDO-1, which in turn accelerates the degradation of Trp through the KP. This not only depletes Trp, which is necessary for serotonin synthesis, but also increases the production of neurotoxic metabolites such as QUIN and 3-HK.
The enzyme kynurenine 3-monooxygenase (KMO), which converts KYN to 3-HK, is another key player in this process. KMO can be induced by pro-inflammatory cytokines, leading to elevated levels of 3-HK. Pharmacological inhibition of KMO or knockout of the KMO gene has been shown to increase levels of KYN and KYNA, suggesting potential therapeutic targets for mitigating the neurotoxic effects of the KP in COVID-19.
Neurological and Psychiatric Implications of KP Dysregulation
The neurological and psychiatric complications associated with COVID-19 are diverse and often severe. Acute COVID-19 infection can lead to a range of neurological symptoms, from headaches and dizziness to more severe conditions such as encephalopathy and strokes. However, the long-term effects, as seen in long COVID, are particularly concerning.
Long COVID is characterized by persistent symptoms that can last for months after the acute infection has resolved. Common neurological symptoms of long COVID include cognitive impairment, often referred to as "brain fog," as well as fatigue, headaches, and mood disturbances. Research has shown that these symptoms are associated with sustained activation of the KP, with elevated levels of neurotoxic metabolites such as QUIN and 3-HK being particularly implicated.
The Role of the Immune System and KP in Long COVID
The interaction between the immune system and the KP is a critical area of research in understanding long COVID. The persistent activation of the KP and the resulting production of neurotoxic metabolites are driven by ongoing inflammation and immune dysregulation. This chronic inflammatory state can lead to the disruption of the blood-brain barrier, allowing neurotoxic metabolites to enter the central nervous system (CNS) and cause further damage.
In addition to direct neurotoxicity, the immune response itself can contribute to neurological symptoms. For instance, IDO-1 activation in immune cells such as dendritic cells and macrophages leads to the production of KYN, which can then activate the aryl hydrocarbon receptor (AhR) in these cells. This activation promotes a tolerogenic phenotype in dendritic cells, leading to the differentiation of regulatory T cells (Treg) and suppressing inflammatory responses. However, in the context of a persistent viral infection like COVID-19, this immune modulation can contribute to chronic inflammation and the ongoing production of neurotoxic KP metabolites.
Therapeutic Implications and Future Research
Understanding the role of the KP in COVID-19 neuropathogenesis opens up potential therapeutic avenues. Inhibitors of KP enzymes, such as IDO-1 and KMO, could help reduce the production of neurotoxic metabolites and mitigate neurological symptoms. Additionally, therapies aimed at modulating the immune response and reducing inflammation could indirectly impact the KP and improve outcomes for patients with long COVID.
Future research should focus on longitudinal studies to track changes in KP metabolites over time in COVID-19 patients. This would help identify biomarkers for predicting which patients are at risk for long COVID and guide the development of targeted interventions. Additionally, exploring the interaction between the KP and other metabolic and immune pathways could provide a more comprehensive understanding of the disease's impact on the CNS.
Conclusion
The research conducted by Macquarie University, the University of Melbourne, and St. Vincent’s Centre for Applied Medical Research has shed light on the critical role of the kynurenine pathway in COVID-19 neuropathogenesis. The activation of the KP and the resulting production of neurotoxic metabolites such as QUIN and 3-HK are significant factors in both the acute and long-term neurological impacts of COVID-19. By continuing to explore the complex interactions between the KP, the immune system, and SARS-CoV-2, researchers can develop more effective treatments and improve the long-term outcomes for patients affected by this multifaceted disease.
The study findings were published in the peer reviewed journal: Infection (springer Link).
https://link.springer.com/article/10.1007/s15010-024-02293-y
For the latest
COVID-19 News, keep on logging to Thailand Medical News.
Read Also:
https://www.thailandmedical.news/news/long-covid-news-decreased-plasma-tryptophan-and-increased-kynurenine-levels-may-be-contributing-factors-to-long-covid-symptoms
https://www.thailandmedical.news/news/breaking-covid-19-news-various-studies-and-case-reports-validate-that-sars-cov-2-can-cause-bipolar-disorder
https://www.thailandmedical.news/news/covid-19-news-sars-cov-2-infections-can-trigger-onset-of-bipolar-disorder