Study Alarmingly Reveals That SARS-CoV-2 Infection Causes Immunodeficiency In Recovered Patients By Downregulating CD19 Expression In B Cells!
Source: Medical News-CD19-SARS-CoV-2 Nov 10, 2021 4 years, 3 months, 6 days, 3 hours, 18 minutes ago
A new multi-country research by scientist from Huazhong University of Science and Technology, Wuhan-China, Third Hospital of Shanxi Medical University, Taiyuan-China, Wuhan Institute of Virology-Chinese Academy of Sciences-China, Karolinska Institute-Sweden, Universidad Autónoma de Chile, University of Ulsan College of Medicine, Seoul-Korea, RIKEN Yokohama Institute, Kanagawa-Japan, The University of Hong Kong and Yangtze University, Jingzhou-China has alarmingly found that SARS-CoV-2 infection causes immunodeficiency in recovered patients by downregulating CD19 expression in B cells via enhancing B-cell metabolism!
It is already known that the SARS-CoV-2 infection causes severe immune disruption. However, it is unclear if disrupted immune regulation still exists and pertains in recovered COVID-19 patients.
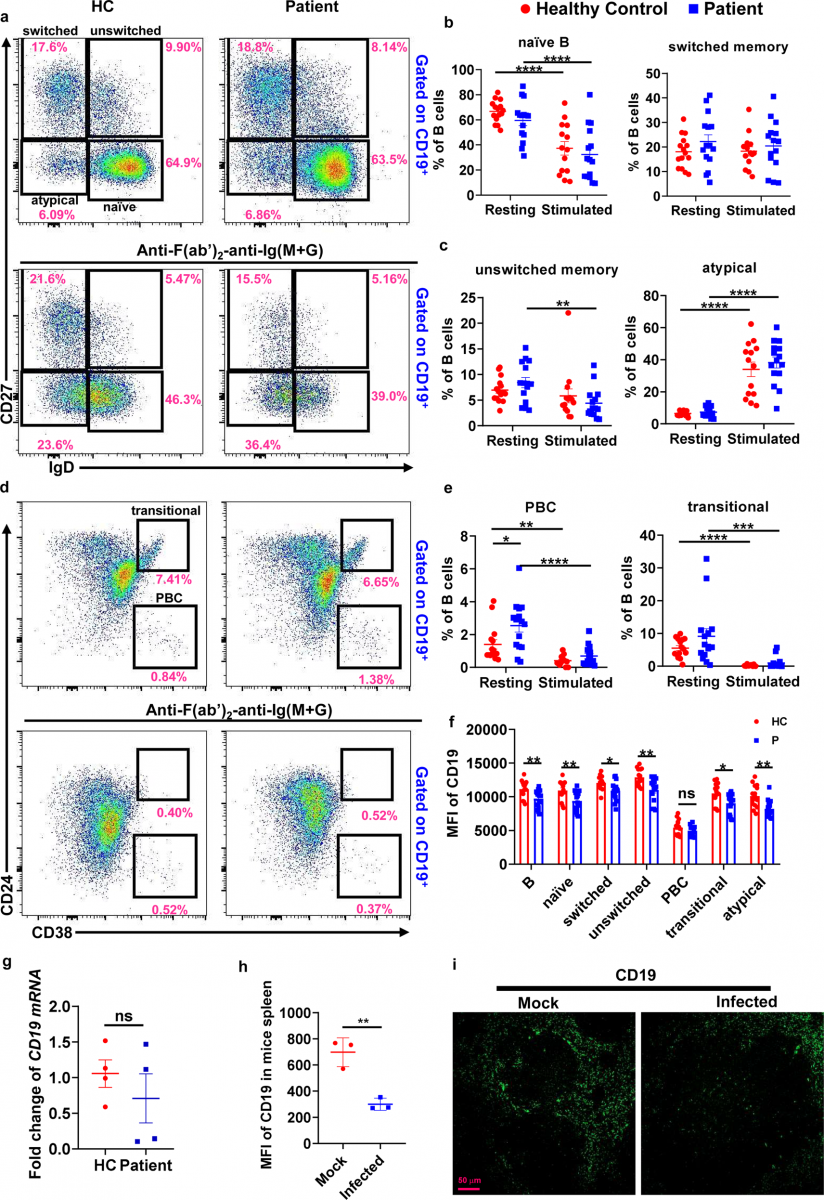
In this new research, the study team characterized the immune phenotype of B cells from 15 recovered COVID-19 patients, and found that healthy controls and recovered patients had similar B-cell populations before and after BCR stimulation, but the frequencies of PBC in patients were significantly increased when compared to healthy controls before stimulation.
However, the percentage of unswitched memory B cells was decreased in recovered patients but not changed in healthy controls upon BCR stimulation.
Shockingly, the study findings revealed that CD19 expression was significantly reduced in almost all the B-cell subsets in recovered patients. Moreover, the BCR signaling and early B-cell response were disrupted upon BCR stimulation.
Mechanistically, the study team found that the reduced CD19 expression was caused by the dysregulation of cell metabolism.
The study findings confirmed that that SARS-CoV-2 infection causes immunodeficiency in recovered patients by downregulating CD19 expression in B cells via enhancing B-cell metabolism, which may provide a new intervention target to cure COVID-19.
The study findings were published in the peer reviewed journal: Signal Transduction And Targeted Therapy (Nature)
https://www.nature.com/articles/s41392-021-00749-3
Numerous past studies have shown that the SARS-CoV-2 infection causes has caused immune disruption in a variety of ways.
Studies have reported that COVID-19 patients had decreased lymphocyte counts and increased counts of myeloid cells in peripheral blood.
https://www.nature.com/articles/s41421-020-0168-9
https://jamanetwork.com/journals/jama/article-abstract/2761044
Many recent reports show lymphopenia with drastically reduced numbers of both CD4+ and CD8+ T cells in moderate and severe COVID-19 cases.
https://jamanetwork.com/journals/jamanetworkopen/article-abstract/2766670
https://academic.oup.com/jid/article/221/11/1762/5813618?login=true
F
low cytometry analysis of PBMCs from symptomatic COVID-19 patients has shown a significant influx of granulocyte-macrophage colony-stimulating factor (GM-CSF)-producing, activated CD4+ T cells and CD14+ HLA-DRlo inflammatory monocytes (IMs).
https://www.sciencedirect.com/science/article/pii/S1931312820302365
https://academic.oup.com/nsr/article/7/6/998/5804736?login=true
Numerous studies have also shown reduced numbers of NK cells in the PBMC of COVID-19 patients, which is associated with the severity of the disease.
https://academic.oup.com/jid/article/221/11/1762/5813618?login=true
https://www.medrxiv.org/content/10.1101/2020.03.05.20031906v1
It is however unclear if the disrupted immune regulation still exists and pertains in recovered patients.
In this research, the study team characterized the immune phenotype of B cells from 15 recovered COVID-19 patients. Healthy control and recovered patients had similar B-cell populations at the resting and stimulated state.
However, the frequencies of PBC in patients were significantly increased when compared to healthy controls before stimulation, and the percentage of unswitched memory B cells was decreased in recovered patients but not changed in healthy controls upon BCR stimulation.
More importantly, the study team found that CD19 expression was significantly reduced in almost all the B-cell subsets in recovered patients.
Corresponding author Dr Zhongxin Lu from the Department of Medical Laboratory, The Central Hospital of Wuhan, Huazhong University of Science and Technology told Thailand
Medical News, “CD19 is one of the members of the B-cell receptor co-complex, consisting of CD19, CD81, CD21, and CD225, which effectively amplifies antigenic signaling via the B-cell receptor (BCR). Thus, although the CD19 expression in recovered COVID-19 patients was mildly reduced within a range of about 10% probably, BCR signaling was largely decreased in B cells from recovered patients upon BCR activation.”
CD19 is a critical regulator of BCR signaling, B-cell development, and humoral immune response.
It was previously reported that CD19 downregulation leads to immunodeficiency by regulating the early activation of memory B cells in Wiskott–Aldrich syndrome patients. https://ashpublications.org/blood/article/128/13/1723/35394/The-early-activation-of-memory-B-cells-from
Shockingly the study findings revealed that the BCR signaling and early B-cell response including B-cell spreading, BCR clustering, and signalosome recruitment was disrupted upon BCR stimulation in recovered patients.
It was found that mechanistically, the reduced CD19 expression is caused by enhanced ROS production, instead of gene transcription, in recovered COVID-19 patients.
The study findings conclude that the immune deficiency in recovered patients is due to the reduced CD19 expression, which dampens the BCR signaling.
Evidence suggests that the metabolic environment plays a major role in directing B-cell fate and function, and changes in oxygen availability and other metabolic alterations profoundly affect B-cell survival, activation, and differentiation.
https://www.jimmunol.org/content/192/8/3626.short
https://www.sciencedirect.com/science/article/abs/pii/S0952791519300810
The study findings showed that among the altered metabolites in the analysis of serum metabolite profiles, the levels of the amino acids L-arginine, L-glutamic acid, L-isoleucine, L-cystine, and L-cysteine were significantly reduced in the serum from recovered COVID-19 patients. These results indicate that the disrupted metabolism may affect B-cell activation and function in recovered patients.
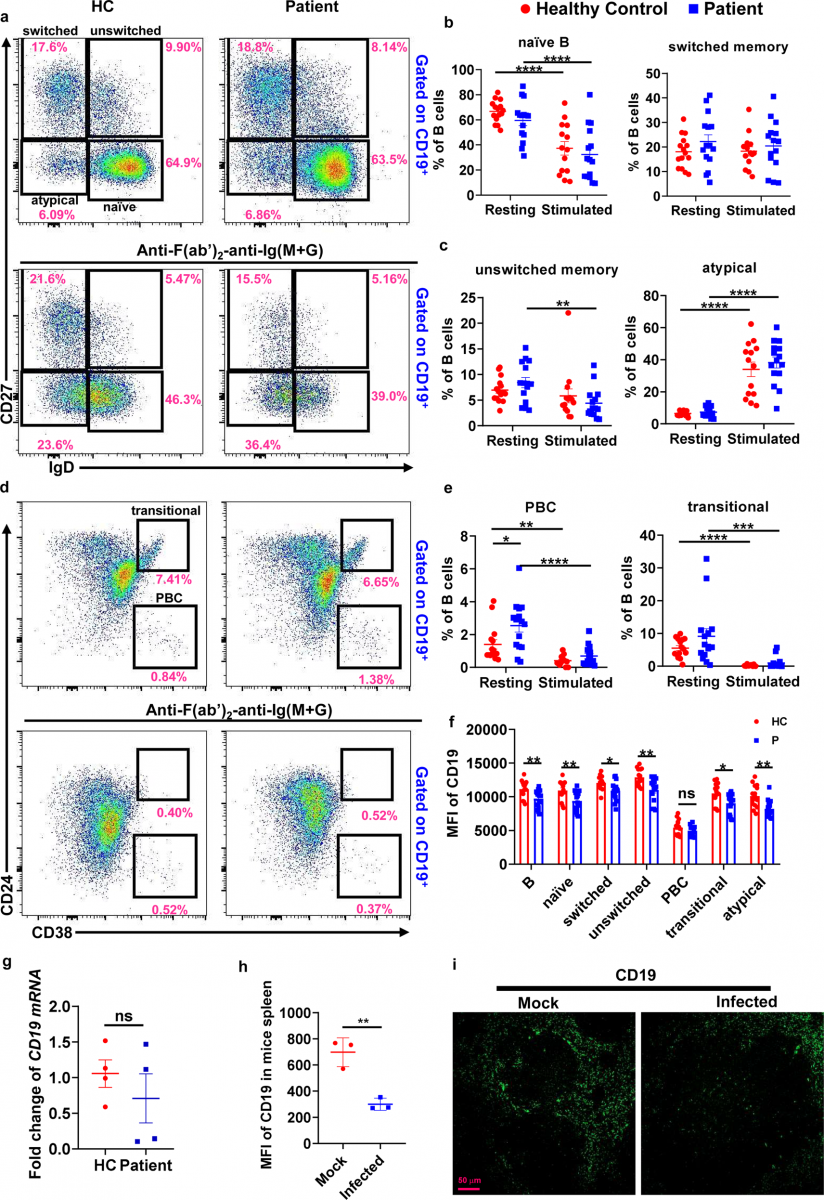 SARS-CoV-2 infection alters the immune phenotype and function of B cells and reduces CD19 expression on B cells from recovered COVID-19 patients. Flow cytometry analysis of the frequencies of naive B cells (naive, CD19+ IgD+CD27−), class-switched B cells (switched, CD19+ IgD−CD27+), unswitched memory B cells (unswitched, CD19+IgD+CD27+), transitional B cells (transitional, CD19+CD24+CD38+), plasma blasts (PBC, CD19+CD38+CD24−) and atypical memory B cells (atypical, CD19+IgD−CD27−) in resting and stimulated PBMCs from COVID-19 recovered patients (n = 14–15) and healthy controls (n = 15). Shown are representative dot plots (a, d) and the average percentages (±SEM) of B-cell subpopulations (b, c, e). Flow cytometry analysis of the MFI of CD19 on total B cells (B, CD19+), naive B cells, class-switched B cells, unswitched memory B cells, transitional B cells, plasma blasts, and atypical memory B cells in resting PBMCs from COVID-19 recovered patients (n = 15) and healthy controls (n = 15). Resting = cells before stimulation, Stimulated = cells after stimulation with 10 µg/ml biotin-F(ab′)2-anti-Ig(M + G) for 24 h (f). RT-PCR analysis of CD19 mRNA levels of B cells from recovered patients (n = 4) and healthy controls (n = 4) (g). Immunofluorescence analysis of CD19 expression in nephritic sections from SARS-CoV-2 infected mice (n = 3) and mock mice (n = 3). Shown are representative images (h, i). Statistical evaluation was performed using the two-tailed Student’s t-test. Statistical significance is indicated using asterisks: *p < 0.05,**p < 0.01, ***p < 0.001, and ****p < 0.0001
SARS-CoV-2 infection alters the immune phenotype and function of B cells and reduces CD19 expression on B cells from recovered COVID-19 patients. Flow cytometry analysis of the frequencies of naive B cells (naive, CD19+ IgD+CD27−), class-switched B cells (switched, CD19+ IgD−CD27+), unswitched memory B cells (unswitched, CD19+IgD+CD27+), transitional B cells (transitional, CD19+CD24+CD38+), plasma blasts (PBC, CD19+CD38+CD24−) and atypical memory B cells (atypical, CD19+IgD−CD27−) in resting and stimulated PBMCs from COVID-19 recovered patients (n = 14–15) and healthy controls (n = 15). Shown are representative dot plots (a, d) and the average percentages (±SEM) of B-cell subpopulations (b, c, e). Flow cytometry analysis of the MFI of CD19 on total B cells (B, CD19+), naive B cells, class-switched B cells, unswitched memory B cells, transitional B cells, plasma blasts, and atypical memory B cells in resting PBMCs from COVID-19 recovered patients (n = 15) and healthy controls (n = 15). Resting = cells before stimulation, Stimulated = cells after stimulation with 10 µg/ml biotin-F(ab′)2-anti-Ig(M + G) for 24 h (f). RT-PCR analysis of CD19 mRNA levels of B cells from recovered patients (n = 4) and healthy controls (n = 4) (g). Immunofluorescence analysis of CD19 expression in nephritic sections from SARS-CoV-2 infected mice (n = 3) and mock mice (n = 3). Shown are representative images (h, i). Statistical evaluation was performed using the two-tailed Student’s t-test. Statistical significance is indicated using asterisks: *p < 0.05,**p < 0.01, ***p < 0.001, and ****p < 0.0001
It is also known that increased mitochondrial ROS production has been shown to result in decreased CD19 expression, which reduces BCR signaling.
https://onlinelibrary.wiley.com/doi/full/10.1002/eji.201646342
The study showed that ROS was found to increase and CD19 expression was decreased, and interestingly, CD19 expression and BCR signaling was rescued partially in recovered patients by using ROS scavenger-NAC.
The study findings are in line with what has been reported and indicate that increased ROS may affect BCR signaling in recovered patients through inhibiting CD19 expression.
Utilizing transcriptome and metabolism analysis, the study team found the genes related to metabolism and metabolism products were dysregulated.
The study team also found that the ROS of B cells in recovered patients was increased, which indicates an increased cell metabolism of B cells in recovered patients.
Past studies reported that metabolite and lipid alterations are shown apparent correlation with the course of disease in these COVID-19 patients, suggesting that the development of COVID-19 affected whole-body metabolism of the patients.
https://academic.oup.com/nsr/article-abstract/7/7/1157/5826189
https://www.sciencedirect.com/science/article/pii/S0092867420306279
It was interestingly found that CD19 expression was rescued partially in recovered patients by using ROS scavenger-NAC.
The study team demonstrated that the increase of the metabolic state causes decreased expression of the critical immune regulator-CD19 and the immunodeficiency state in recovered patients.
Furthermore, the study team found that the CD19 expression was also reduced in the spleen of infected mice with SARS-CoV-2. Hence the team says that it can be inferred that CD19 expression may be reduced in infected patients as well.
The team said that it could be interesting to examine the CD19 expression in mild and severely infected patients and the metabolism state of B cells.
Also, the team said that the correlation between the CD19 expression and the different metabolism states of B cells is worthy to pursue.
More excitingly, the correction of the increased ROS in B cells rescued the CD19 expression and BCR signaling, which may correct the immune state in recovered patients. It is unknown whether the recovered patients having reduced CD19 expression are more susceptible to be re-infected by SARS-CoV-2. If it is true, the metabolism regulator such as NAC may have a potential clinical application on the prevention of second infection of recovered patients.
Though the study team found the decreased CD19 expression, the level of CD19 mRNA had no change in B cells from recovered patients, which indicates that SARS-CoV-2 infection may reduce the CD19 levels in the period of post-transcriptional translation.
The team also checked several molecules in the BCR signaling pathway from RNA-Seq, but did not find the differences of CD19 mRNA and molecules in the BCR signaling pathway between HC and patients. That’s the reason why the BCR signaling pathway didn’t appear in the KEGG enriched signaling pathways.
The current omics data were analyzed for unstimulated B cells; however, results of the B-cell experiment in vitro were shown when the B cells were activated with F(ab′)2-anti-human Ig (M + G). Therefore, the omics data seem to not effectively match the results of the B-cell experiment in vitro. It would be interesting to analyze the omics data from B cells activated with F(ab′)2-anti-human Ig (M + G) said the study team.
Importantly, as bacterial and fungal infections are common complications in patients with viral pneumonia and lead to increased mortality. Analyzing the signaling properties of B cells from COVID-19 patients would help to assess whether a COVID-19 infection renders an individual more susceptible to other diseases.
A better understanding of how metabolic abnormalities observed in patient serum affect B-cell signaling could inspire the development of new treatment strategies targeting specific metabolic pathways. Different compounds altering cell metabolism and the redox state are currently tested in pre-clinical and clinical studies to treat autoimmune disorders and could also be exploited to dampen an overactive immune response during a viral infection.
https://onlinelibrary.wiley.com/doi/full/10.1002/art.34502
https://www.science.org/doi/abs/10.1126/scitranslmed.aaa0835
https://onlinelibrary.wiley.com/doi/full/10.1002/art.39296
For the latest
SARS-CoV-2 Research, keep on logging to Thailand Medical News.