Ongoing Breathing Issues in Long COVID Might Be Tied to IgA Autoimmunity and Hidden Clotting Dysfunction
Nikhil Prasad Fact checked by:Thailand Medical News Team Jun 01, 2025 9 months, 3 days, 19 hours, 55 minutes ago
Thailand Medical News: Doctors and scientists from NYU Grossman School of Medicine have uncovered potential connections between the immune system and abnormal blood clotting in patients suffering from Long COVID, or what’s officially called Post-Acute Sequelae of SARS-CoV-2 infection (PASC). The findings come from a detailed case-control study exploring why some individuals continue to experience breathing difficulties long after recovering from COVID-19.
 Ongoing Breathing Issues in Long COVID Might Be Tied to IgA Autoimmunity and Hidden Clotting Dysfunction
Ongoing Breathing Issues in Long COVID Might Be Tied to IgA Autoimmunity and Hidden Clotting Dysfunction
In this
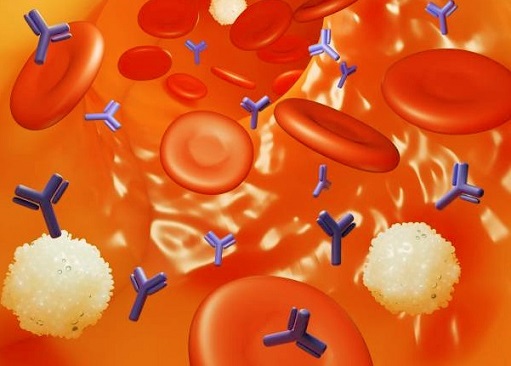
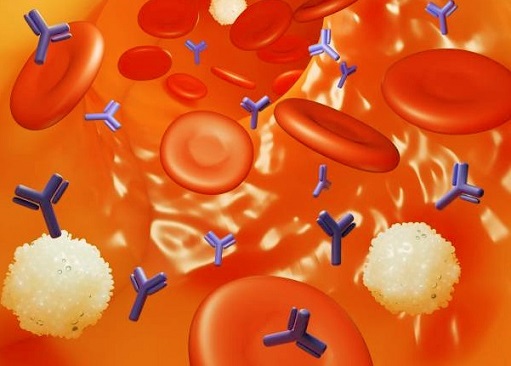
Thailand Medical News report, the researchers focused on the role of a specific type of immune protein called Immunoglobulin A (IgA) and how it may influence both respiratory symptoms and the body’s clotting systems. Their aim was to better understand the biological reasons behind persistent symptoms such as shortness of breath, which affect a large percentage of Long COVID sufferers.
Who Was Studied and What Was Measured
The study included 20 individuals with Long COVID who still had breathing problems and compared them with 20 people who had recovered from COVID-19 without any lasting symptoms. All participants had previously tested positive for COVID-19 and had similar age, sex, and health backgrounds. The researchers carried out blood tests, immune system assessments, and nuclear imaging of the lungs using a special type of scan known as SPECT-CT. They also evaluated blood clotting using advanced tools like thromboelastography (TEG).
Importantly, all participants with Long COVID had respiratory complaints such as breathlessness and low oxygen levels. Many also experienced dizziness, abnormal heart rhythms, and even cognitive issues. Their quality of life was markedly lower than the control group, as measured by validated health surveys.
What the Tests Revealed
Surprisingly, the results showed that lower levels of total IgA in the blood were actually linked with more severe respiratory symptoms in Long COVID patients. This is counterintuitive because autoimmune issues usually involve higher levels of antibodies, not lower ones. Even more intriguing, the researchers found that IgA levels were directly connected to blood clotting strength—specifically to the amount of fibrinogen (a clot-forming protein) and the stiffness of the resulting clots.
This means that patients with reduced IgA had both more breathing symptoms and weaker clot formation. This may indicate that IgA, rather than just attacking the body in classic autoimmunity, plays a complex and perhaps protective role in regulating blood flow and lung function after COVID-19.
The researchers also measured how much IgA was targeting specific lung cells, including microvascular endothelial cells (which line blood vessels) and epithelial cells (which form the lung’s surface lining). Again, lower levels of these targeted IgA antibodies were found in the Long COVID group, especially those binding to blood vessel cells. This reinf
orces the idea that a lack, rather than an excess, of certain immune responses might be contributing to ongoing symptoms.
Imaging and Clotting Tests Offered Mixed Clues
When they looked at SPECT-CT scan results, 25% of Long COVID patients showed signs of small blood flow problems in the lungs compared to just 10% of healthy controls. Although this difference wasn’t statistically significant due to the small sample size, it hints that microvascular dysfunction might be more common in Long COVID. Some of these abnormalities were accompanied by air-trapping in the lungs—a sign that small airways could be affected.
However, TEG results, which evaluate how blood clots in real time, didn’t show strong differences between the groups. This suggests that abnormalities seen in Long COVID might not show up in routine blood clotting tests and might involve complex tissue-level processes not captured in standard evaluations.
Why This Matters
These findings suggest that Long COVID is not simply a continuation of the initial viral illness but may involve long-term immune imbalance and microvascular injury. The unique role of IgA—typically involved in mucosal defense, like in the lungs—appears to be central to this process. Rather than being elevated, its reduced presence and specific targeting in the body might be leading to both inflammation and dysfunctional clotting.
While the study sample was small and cannot draw firm conclusions, it opens new avenues for diagnosing and treating Long COVID. For instance, measuring specific types of IgA and clotting parameters could help identify which patients are at higher risk for persistent breathing issues and other complications. Moreover, treatments that stabilize IgA levels or improve microvascular blood flow might offer relief to those who remain sick for months or even years after their initial infection.
Conclusion
This study highlights the strange and unexpected role that low levels of IgA antibodies might play in the lingering symptoms of Long COVID. Rather than causing direct damage, the lack of appropriate immune targeting and regulation could be contributing to blood flow issues and weakened lung function. The research also underscores the complexity of Long COVID and the need for more sensitive diagnostic tools beyond standard blood tests or scans. Understanding the relationship between immunity and blood clotting may be essential in developing future therapies for this growing patient population.
The study findings were published in the peer reviewed journal: Frontiers in Immunology
https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1589559/full
For the latest COVID-19 News, keep on logging to
Thailand Medical News
Read Also:
https://www.thailandmedical.news/news/sars-cov-2-induced-igg-autoantibodies-are-targeting-various-immune-cells-and-also-proteins-in-various-organs
https://www.thailandmedical.news/news/study-shows-that-individuals-who-have-recovered-from-covid-19-are-more-likely-to-develop-antinuclear-antibodies
https://www.thailandmedical.news/news/doctors-from-slovakia-warn-that-even-mild-covid-19-can-trigger-rare-autoimmune-brain-disorder
https://www.thailandmedical.news/articles/coronavirus
https://www.thailandmedical.news/pages/thailand_doctors_listings