Nikhil Prasad Fact checked by:Thailand Medical News Team Sep 18, 2025 4 months, 2 weeks, 1 day, 14 hours, 31 minutes ago
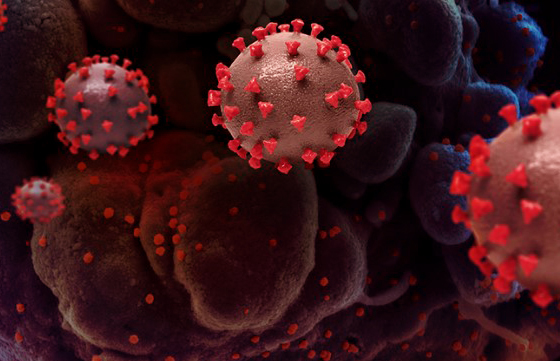
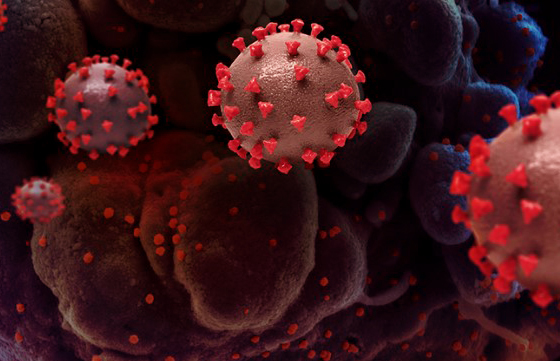
Medical News: Researchers from the Department of Biomedicine, Neurosciences and Advanced Diagnostics at the University of Palermo and the Department of Medicine and Surgery at Kore University of Enna have uncovered how a common cellular protein called heat shock protein 60 (Hsp60) could play a central role in COVID-19 complications. Their work shows how Hsp60 is linked not only to inflammation and blood vessel damage but also to the dangerous possibility of autoimmunity. This
Medical News report takes a closer look at their findings.
 Hidden HSP60 Connection to Long COVID and Autoimmunity
What is Hsp60
Hidden HSP60 Connection to Long COVID and Autoimmunity
What is Hsp60
Hsp60 is a protein normally responsible for helping other proteins fold correctly and protecting cells under stress. Under normal conditions, it works inside mitochondria, the cell’s power plants. However, when cells are damaged, Hsp60 can be released into the bloodstream where it interacts with the immune system. Instead of helping, it can set off harmful inflammatory signals and trigger reactions that look very similar to what happens in COVID-19 patients.
Hsp60 and COVID19 Inflammation
When SARS-CoV-2 infects the body, the immune system goes into overdrive. Studies show that extracellular Hsp60 can bind to immune receptors such as Toll-like receptor 4, stimulating the release of strong inflammatory molecules like TNF-α, IL-6, and IL-1β. This reaction fuels the dangerous cytokine storm seen in severe COVID-19 cases, which can damage lungs, the heart, and other organs.
Autoimmunity and Molecular Mimicry
One of the most concerning discoveries is that Hsp60 shares molecular patterns, called epitopes, with SARS-CoV-2 proteins. This phenomenon, known as molecular mimicry, can trick the immune system into attacking its own cells after fighting the virus. Such a process has been connected to disorders like Guillain-Barré syndrome, autoimmune thyroiditis, vasculitis, and even central nervous system demyelination. Reports of patients developing neurological issues and nerve inflammation after COVID-19 highlight this link.
Endothelial Damage and Clotting Risks
The research also highlights that Hsp60 may relocate to the surface of stressed blood vessel cells. Once exposed, it can act as a false alarm, making the immune system attack blood vessels. This leads to inflammation, blood clot formation, and in severe cases, multi-organ failure. This mechanism helps explain why so many COVID-19 patients suffered vascular complications, strokes, and thromboembolic events.
Double Edged Role in Cancer
Interestingly, while Hsp60-driven mimicry can cause autoimmunity, it may also generate anti-tumor responses. Some scientists have reported that in rare cases, patients with cancers such as colorectal cancer showed tumor reduction after COVID-19 infection, possibly because the immune system also attacked tumor cells carrying similar markers.
Conclusion
This research underline
s how Hsp60 plays a dangerous double role in COVID-19. On one side, it fuels inflammation, vessel damage, and autoimmunity, leading to long-lasting health problems after infection. On the other side, it might help trigger protective immunity against cancer. Understanding this balance will be essential for designing future treatments and safer vaccines. Hsp60 may serve as both a warning marker of severe disease and a therapeutic target to reduce complications.
The study findings were published in the peer reviewed journal: Biology.
https://www.mdpi.com/2079-7737/14/9/1281
For the latest on Long COVID, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/rising-concern-over-surge-in-anti-mda5-dermatomyositis-cases-following-covid-19
https://www.thailandmedical.news/news/individuals-exposed-to-covid-19-age-faster-at-a-molecular-level-and-face-higher-risk-of-age-related-diseases-and-shorter-lifespans
https://www.thailandmedical.news/news/covid-19-triggers-dangerous-brain-pressure-leading-to-headaches-seen-in-long-covid