Nikhil Prasad Fact checked by:Thailand Medical News Team Feb 18, 2024 2 years, 1 week, 2 days, 4 hours, 29 minutes ago
COVID-19 News: The ongoing global pandemic caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has led to widespread morbidity and mortality, with coronavirus disease 2019 (COVID-19) affecting millions worldwide. While the primary target of SARS-CoV-2 is the respiratory system, emerging evidence highlights its ability to infect various organs, including the liver, leading to hepatic dysfunction observed in over 50% of COVID-19 patients. This multi-organ involvement underscores the complex pathogenesis of the virus, prompting researchers to investigate alternative receptors beyond the well-known angiotensin I converting enzyme 2 (ACE2) for SARS-CoV-2 entry into host cells.
 Asialoglycoprotein receptor 1 promotes SARS-CoV-2 infection of human normal hepatocytes
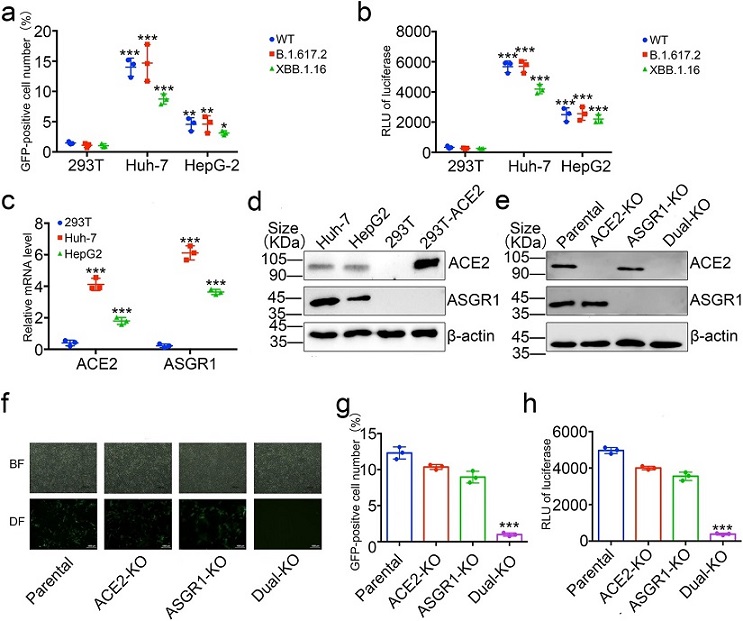
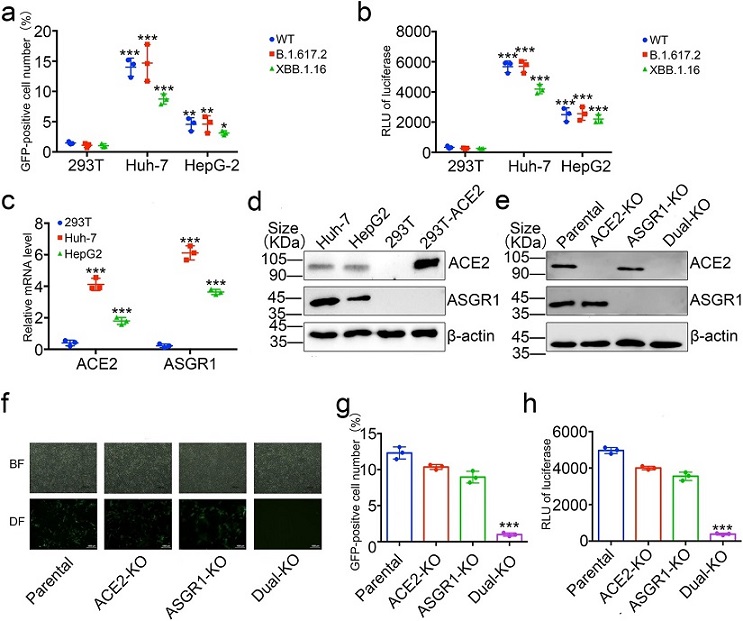
SARS-CoV-2 pseudovirus can infect liver cell lines through ASGR1 in vitro. HEK293T, Huh-7, and HepG2 cells were infected with the GFP-labeled and luciferase SARS-CoV-2 pseudotype virus with the Spike protein of wild type, XBB.1.16 or B.1.617.2, detect the expression levels of GFP by cell flow cytometer (a), and luciferase by microplate (b) at 72 h post-infection. c ACE2 and ASGR1 expressions were measured by qPCR. The intracellular RNA of 293 T, Huh-7, and HepG2 cells was extracted, and after reverse transcription, the corresponding primers were used to amplify ACE2, ASGR1, and GAPDH respectively. The expression levels of ACE2 or ASGR1 were finally normalized by GAPDH. d ACE2 and ASSGR1 expressions were measured by Western blot. Western blot of cell lysate of 293T, Huh-7, and HepG2 cells with anti-ACE2 or anti-ASGR1 was performed to identify expression of ACE2 or ASGR1 protein. e ACE2 and ASSGR1 expressions were measured by Western blot in Huh-7 cells with knockout of ASGR1, ACE2, or both with anti-ACE2 or anti-ASGR1. f–h SARS-CoV-2 pseudovirus with wild-type Spike can infect Huh-7 cells through ACE2 or ASGR1. Huh-7 cells with knockout of ASGR1, ACE2, or both, were infected with the GFP-labeled and luciferase SARS-CoV-2 pseudotype virus with wild type Spike and visualized by microscopy (f), expression levels of GFP by cell flow cytometer (g), and detection of luciferase by microplate (h) at 72 h post-infection. Scale bars, 1000 μm.
Asialoglycoprotein receptor 1 promotes SARS-CoV-2 infection of human normal hepatocytes
SARS-CoV-2 pseudovirus can infect liver cell lines through ASGR1 in vitro. HEK293T, Huh-7, and HepG2 cells were infected with the GFP-labeled and luciferase SARS-CoV-2 pseudotype virus with the Spike protein of wild type, XBB.1.16 or B.1.617.2, detect the expression levels of GFP by cell flow cytometer (a), and luciferase by microplate (b) at 72 h post-infection. c ACE2 and ASGR1 expressions were measured by qPCR. The intracellular RNA of 293 T, Huh-7, and HepG2 cells was extracted, and after reverse transcription, the corresponding primers were used to amplify ACE2, ASGR1, and GAPDH respectively. The expression levels of ACE2 or ASGR1 were finally normalized by GAPDH. d ACE2 and ASSGR1 expressions were measured by Western blot. Western blot of cell lysate of 293T, Huh-7, and HepG2 cells with anti-ACE2 or anti-ASGR1 was performed to identify expression of ACE2 or ASGR1 protein. e ACE2 and ASSGR1 expressions were measured by Western blot in Huh-7 cells with knockout of ASGR1, ACE2, or both with anti-ACE2 or anti-ASGR1. f–h SARS-CoV-2 pseudovirus with wild-type Spike can infect Huh-7 cells through ACE2 or ASGR1. Huh-7 cells with knockout of ASGR1, ACE2, or both, were infected with the GFP-labeled and luciferase SARS-CoV-2 pseudotype virus with wild type Spike and visualized by microscopy (f), expression levels of GFP by cell flow cytometer (g), and detection of luciferase by microplate (h) at 72 h post-infection. Scale bars, 1000 μm.
Liver injury in COVID-19 patients has been linked to both systemic cytokine responses and direct viral infection of hepatocytes. Recent autopsies and electron microscopy studies have confirmed the presence of intracellular virus particles within hepatocytes, suggesting a direct cytopathic effect of SARS-CoV-2 in the liver. Surprisingly, hepatocytes express ACE2 at extremely low levels, raising questions about the mechanisms facilitating SARS-CoV-2 infection in the liver.
In this study conducted at Fudan University in Shanghai, China and covered in this
COVID-19 News report, researchers aimed to explore alternative receptors in hepatocytes that might facilitate SARS-CoV-2 entry. Using a genome-wide CRISPR-Cas9 activation library screenin
g, the team identified Asialoglycoprotein receptor 1 (ASGR1) as a potential receptor for SARS-CoV-2. This finding adds a new dimension to our understanding of the virus's cellular tropism and opens avenues for therapeutic interventions.
Thailand
Medical News had already covered numerous past studies as to how the SARS-CoV-2 virus can directly or indirectly affect the liver.
https://www.thailandmedical.news/news/covid-19-news-scientists-unveil-molecular-mechanisms-underlying-sars-cov-2-hepatotropism-and-liver-damage
https://www.thailandmedical.news/news/breaking-news-brazilian-study-shockingly-finds-that-sars-cov-2-directly-infects-liver-cells-or-hepatocytes-to-cause-hyperglycemia
https://www.thailandmedical.news/news/argentinian-researchers-warn-that-sars-cov-2-could-be-a-hepatotropic-virus-that-also-manipulates-glucose-metabolism
https://www.thailandmedical.news/news/new-york-clinicians-sound-the-alarm-covid-19-asymptomatic-individuals-can-suffer-acute-liver-injury
https://www.thailandmedical.news/news/covid-19-research-the-detrimental-effects-of-tnf%CE%B1-on-liver-during-sars-cov-2-infection-and-its-impact-on-patient-survival
https://www.thailandmedical.news/news/breaking-covid-19-news-brazil-study-shows-that-most-long-covid-individuals-continue-to-sustain-damaged-liver-functions-up-to-20-months
https://www.thailandmedical.news/news/covid-19-news-fatty-acids-impact-ace2-receptor-expression-in-metabolic-dysfunction-associated-steatotic-liver-disease
https://www.thailandmedical.news/news/breaking-covid-19-news-scientists-from-university-of-texas-warn-that-sars-cov-2-can-also-cause-seronegative-autoimmune-hepatitis-in-adults
https://www.thailandmedical.news/news/covid-19-news-german-researchers-warn-that-sclerosing-cholangitis-emerging-as-a-consequence-of-severe-covid-19-infection
https://www.thailandmedical.news/news/coronavirus-news-german-study-confirms-that-sars-cov-2-coronavirus-can-invade-and-damage-the-liver
https://www.thailandmedical.news/news/breaking-covid-19-research-studies-warn-of-high-prevalence-of-liver-injury-in-covid-19-patients
https://www.thailandmedical.news/news/covid-19-research-university-of-bristol-researchers-warn-that-liver-complications-are-common-in-covid-19-patients
https://www.thailandmedical.news/news/breaking-more-emerging-chinese-research-studies-shows-that-the-sars-cov-2-coronavirus-also-attacks-the-kidneys,-pancreas-and-liver
https://www.thailandmedical.news/news/breaking-covid-19-news-sars-cov-2-that-causes-liver-impairment-in-many-also-cause-hypoalbuminemia
https://www.thailandmedical.news/news/breaking-sars-cov-2-impairs-lipid-metabolic-and-autophagic-pathways,-causing-damage-to-heart,-liver-and-kidneys-the-phytochemical-trigonelline-helps
https://www.thailandmedical.news/news/researchers-alarmingly-find-that-metabolic-associated-fatty-liver-disease-mafld-may-be-a-prevalent-long-covid-manifestation
https://www.thailandmedical.news/news/breaking-sars-cov-2-infection-induces-increase-of-gp73-that-causes-dysglycaemia-increased-gp73-could-also-imply-future-liver-disease-and-liver-cancer
https://www.thailandmedical.news/news/breaking-study-finds-that-upregulated-interleukin-6-drives-development-of-rare-liver-cancers-covid-19-infections-causes-elevated-il-6-levels-in-many
https://www.thailandmedical.news/news/are-the-new-sars-cov-2-variants-circulating-in-europe-more-neuropathogenic-with-a-modified-pathogenesis-brain-and-liver-issues-on-the-rise
https://www.thailandmedical.news/news/belgium-researchers-warn-that-more-hospitalized-covid-19-patients-are-manifesting-a-rare-chronic-liver-disease-known-as-sclerosing-cholangitis-could-b
Hepatic or liver damage may be associated with COVID-19 due to direct injury of the viral infection to the liver cells, delayed resolution of inflammation, and viral persistence.
https://pubmed.ncbi.nlm.nih.gov/32489653/
https://pubmed.ncbi.nlm.nih.gov/35105985/
Numerous studies have reported changes in serum markers in long-term COVID, including inflammatory (C-reactive protein) and liver markers (alanine aminotransferase [ALT] and aspartate aminotransferase [AST]).
https://pubmed.ncbi.nlm.nih.gov/33172844/
https://pubmed.ncbi.nlm.nih.gov/33887749/
https://pubmed.ncbi.nlm.nih.gov/33347790/
https://pubmed.ncbi.nlm.nih.gov/33532785/
ASGR1 as a Candidate Receptor
Asialoglycoprotein receptor 1 (ASGR1) has previously been implicated in promoting the entry of hepatitis B virus (HBV) into human hepatocytes. Given its high expression in hepatocytes, ASGR1 has also been explored as a potential target for liver cancer treatment. However, its role in SARS-CoV-2 infection was not clear until this study. The researchers conducted a genome-wide CRISPR-Cas9 activation library screening using HeLa cells, which have low levels of ACE2, and identified ASGR1 as a promoter of SARS-CoV-2 pseudovirus infection.
To validate the role of ASGR1 in SARS-CoV-2 infection, the team employed various cell lines, including liver-derived cell lines Huh-7 and HepG2. They found that SARS-CoV-2 pseudovirus could infect these cells, and the infection was significantly reduced when ASGR1 was knocked out. Further experiments in immortalized hepatocyte cell line THLE-2 and primary hepatic parenchymal cells, which express low levels of ACE2, confirmed successful SARS-CoV-2 pseudovirus infection. However, treatment with ASGR1 antibody or siRNA targeting ASGR1 led to a significant drop in the infection rate, strongly suggesting that ASGR1 facilitates SARS-CoV-2 infection in hepatic parenchymal cells.
Interaction between ASGR1 and Spike Protein
The study delved into the molecular interactions between ASGR1 and the viral Spike protein. Confirming the physical interaction between ASGR1 and Spike protein, the researchers found that ASGR1 could bind to both the receptor binding domain (RBD) and the N-terminal domain (NTD) of the Spike protein. Notably, the binding affinity of ASGR1 with NTD was higher than that with RBD. Competitive binding experiments further revealed that ASGR1 could disrupt the interaction between ACE2 and RBD, suggesting a potential competition between ASGR1 and ACE2 for binding to SARS-CoV-2.
Confirmation in Primary Hepatocytes
To establish the physiological relevance of ASGR1 as a receptor for SARS-CoV-2, the researchers investigated primary hepatocytes. Live SARS-CoV-2 was detected in primary hepatocytes, confirming the virus's ability to infect these cells. Knockdown of ASGR1 using siRNA significantly reduced the infection efficiency, providing further evidence that ASGR1 is the primary receptor for SARS-CoV-2 in primary hepatocytes.
Role of ASGR1 in Non-Alcoholic Fatty Liver Disease
Considering the prevalence of non-alcoholic fatty liver disease (NAFLD) in COVID-19 patients with liver involvement, the study explored the impact of SARS-CoV-2 infection in the context of NAFLD. Using a NAFLD cell model, the researchers observed an increased expression of ACE2 in hepatocytes, indicating a potential mechanism for enhanced SARS-CoV-2 infection in NAFLD. This finding aligns with clinical observations of elevated ACE2 levels in liver diseases.
Therapeutic Implications
The identification of ASGR1 as a key receptor for SARS-CoV-2 in hepatocytes raises intriguing therapeutic possibilities. Soluble ASGR1 protein was employed to inhibit SARS-CoV-2 pseudovirus infection in hepatocytes and other susceptible cells expressing ACE2. The soluble ASGR1 protein demonstrated an inhibitory effect on SARS-CoV-2 infection in a dose-dependent manner, suggesting its potential as a therapeutic agent. Comparisons with known ACE2 inhibitors, A779 and ursodeoxycholic acid (UDCA), revealed the superior inhibitory effect of soluble ASGR1 protein.
Conclusion
In conclusion, this groundbreaking study sheds light on ASGR1 as a novel receptor for SARS-CoV-2 in hepatocytes. The findings not only expand our understanding of the virus's cellular tropism but also offer potential therapeutic avenues. The role of ASGR1 in facilitating SARS-CoV-2 entry into liver cells, particularly in the context of liver diseases such as NAFLD, adds complexity to the pathogenesis of COVID-19. As research continues, further exploration of ASGR1 as a therapeutic target may pave the way for innovative treatments to mitigate liver damage associated with SARS-CoV-2 infection. The study underscores the importance of considering alternative receptors beyond ACE2 in the intricate interplay between SARS-CoV-2 and host cells
The study findings were published in the peer reviewed journal: Signal Transduction And Targeted Therapy (Nature).
https://www.nature.com/articles/s41392-024-01754-y
For the latest
COVID-19 News, keep on logging to Thailand Medical News.