Breaking! University Of Alabama Discovers That Mild COVID-19 Causes Brain Temperature Elevation And Free Water Increases In The Brain!
Nikhil Prasad Fact checked by:Thailand Medical News Team Mar 31, 2024 1 year, 10 months, 1 week, 6 days, 23 hours, 19 minutes ago
COVID-19 News: The ongoing COVID-19 pandemic has brought to light various facets of the virus's impact on human health, including the often-overlooked neurological consequences. While severe cases of COVID-19 have been extensively studied for their neurological manifestations, including strokes, encephalopathy, and acute respiratory distress syndrome, the effects of mild COVID-19 infections on brain health have received less attention until recently. In this
COVID-19 News report, we delve into a new study by researchers from the University of Alabama at Birmingham (UAB)-USA, that explores the intricate details of brain temperature elevation and free water increases (edema) observed in individuals with mild COVID-19, shedding light on the potential long-term neurological sequelae of the disease.
 Mild COVID-19 Causes Brain Temperature Elevation And Free Water Increases In The Brain
Mild COVID-19 Causes Brain Temperature Elevation And Free Water Increases In The Brain.
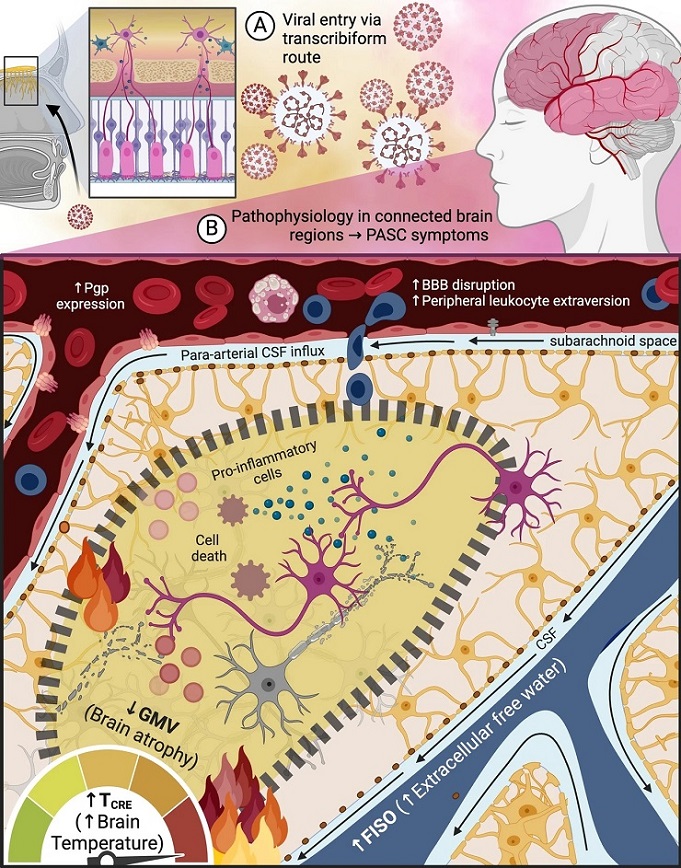
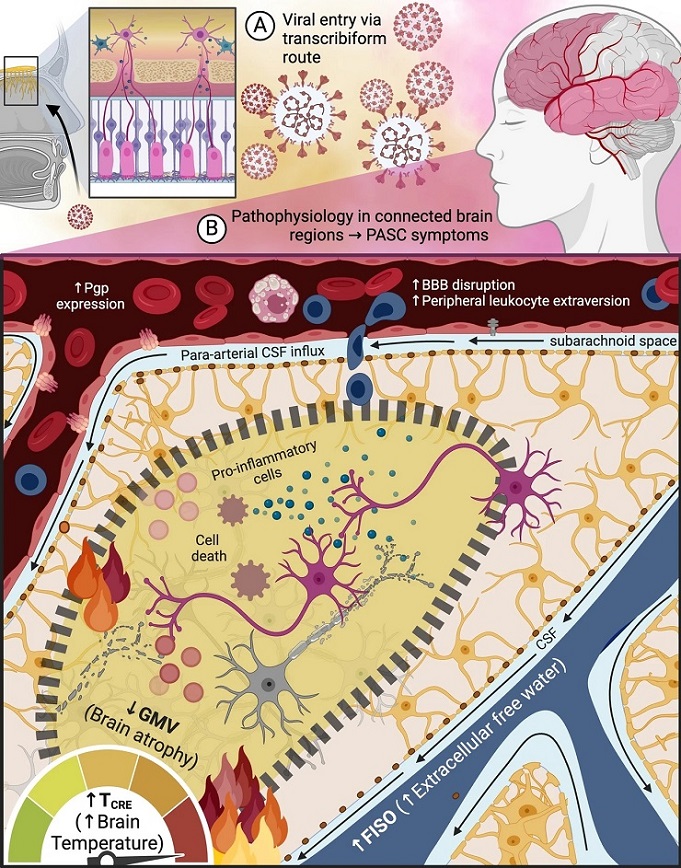
The potential entry of the SARS-Cov-2 virus into the brain through the transcribiform pathway may contribute to neuroinflammation during both the (A) acute and (B) chronic phases of mild COVID-19 infection. This hypothesis suggests that viral entry could activate sustained microglial cell activation, leading to cell death and edema. These changes may manifest as increased brain temperature (TCRE) and extracellular free water (fractional isotropic volume fraction or FISO), which are proposed indicators of neuroinflammation. While the imaging data in this study support this hypothesis, the study design is not suitable for establishing causal relationships. Future investigations should explore the potential connection between SARS-Cov-2 and neuroinflammation, as well as the mechanisms underlying the virus's interaction with the brain and the long-term effects of COVID-19 on neurological function. This figure was created using Biorender.com. MRSI-t volumetric magnetic resonance spectroscopic imaging and thermometry, CRE creatine, TCRE brain temperature measured by MRSI-t with CRE as the reference metabolite, FISO fractional isotropic volume fraction, GMV grey matter volume, BBB blood brain barrier, Pgp P-glycoprotein, CSF cerebrospinal fluid.
Understanding the Impact of Mild COVID-19 on Brain Health
As the pandemic progressed, it became increasingly evident that even individuals with mild or asymptomatic COVID-19 infections could experience lingering neurological symptoms. These symptoms, collectively referred to as "brain fog," encompass a range of cognitive impairments, mood changes, and sensory abnormalities. Notably, a significant subset of individuals with mild COVID-19 continues to experience these symptoms beyond the acute phase of the infection, leading to the recognition of a condition known as post-acute sequelae of COVID-19 (PASC) or long COVID.
Neuroimaging studies have emerged as crucial tools in unraveling the underlying mechanisms of PASC, particularly in individuals with mild COVID-19. While early studies primarily focused on macroscopic abnormalities in hospitalized patients, recent research has shifted toward
s investigating subtle, long-lasting changes in brain structure and function that may underlie persistent neurological symptoms.
Brain Temperature Elevation: A Biomarker of Neuroinflammation
One of the novel aspects of our study is the exploration of brain temperature changes as a potential biomarker of neuroinflammation in individuals with mild COVID-19. Neuroinflammation, characterized by immune cell activation and cytokine release in the brain, has been implicated in various neurological disorders, including Alzheimer's disease, multiple sclerosis, and now, post-COVID neurological sequelae.
In the investigation, the study team utilized magnetic resonance spectroscopic imaging and thermometry (MRSI-t) to map brain temperature changes in participants before and after mild COVID-19 infection. The rationale behind using brain temperature as a biomarker lies in the fact that neuroinflammatory processes often lead to localized increases in brain temperature due to impaired cooling mechanisms and increased metabolic activity in affected brain regions.
The study findings revealed significant post-COVID-19 brain temperature elevations in structures associated with olfactory, cognitive, and memory processing. Notably, the left olfactory tubercle exhibited the largest temperature increase, suggesting a potential link between neuroinflammation and chronic olfactory dysfunction in PASC. These temperature elevations, beyond the typical 0.5-1°C difference from core body temperature, indicate ongoing inflammatory processes that may contribute to persistent neurological symptoms.
Free Water Increases and Edema in Brain Regions
In addition to brain temperature changes, the study also investigated free water increases, indicative of edema or swelling, in the brain regions of individuals with mild COVID-19. Edema is a common consequence of neuroinflammation and can disrupt neural circuits, leading to functional impairments.
Using neurite orientation dispersion and density imaging (NODDI), the study team observed significant post-COVID-19 increases in free water content in regions connected to the olfactory cortex, frontal lobes, and cerebellum. These findings suggest widespread neuroinflammatory changes affecting both cortical and subcortical structures involved in various cognitive and sensory processes.
The olfactory cortex, particularly the primary olfactory cortex and related limbic structures, showed prominent free water increases, aligning with our brain temperature findings and the reported olfactory dysfunction in individuals with PASC. The interplay between brain temperature elevation and edema underscores the complex neurobiological consequences of mild COVID-19 on brain health.
Implications for Understanding PASC and Long-Term Neurological Sequelae
The comprehensive analysis provides valuable insights into the pathophysiology of PASC, especially in individuals with mild COVID-19 infections. The observed brain temperature elevations and free water increases point towards ongoing neuroinflammatory processes that may contribute to the persistence of cognitive, mood, and sensory symptoms seen in PASC.
Furthermore, the study findings highlight the importance of long-term monitoring and personalized interventions for individuals recovering from mild COVID-19. Early detection of neuroinflammatory changes through advanced neuroimaging techniques could aid in targeted therapeutic strategies aimed at mitigating the long-term neurological sequelae of the disease.
Future Directions and Research Implications
While the study significantly advances our understanding of mild COVID-19's impact on brain health, several avenues for future research merit exploration. Longitudinal studies tracking brain temperature, free water content, and clinical outcomes over extended periods are essential to unraveling the trajectory of PASC and identifying predictive biomarkers of neurological recovery or deterioration.
Moreover, investigating the effects of potential treatments or interventions on neuroinflammatory markers in individuals with PASC could pave the way for tailored therapeutic approaches. Collaborative efforts between neuroscientists, clinicians, and public health experts are crucial in addressing the multifaceted challenges posed by COVID-19-related neurological complications.
Conclusion
In conclusion, the in-depth analysis of brain temperature elevation and free water changes in individuals with mild COVID-19 underscores the complex interplay between neuroinflammation and persistent neurological symptoms. By leveraging advanced neuroimaging techniques, we have illuminated potential biomarkers of PASC and laid the groundwork for targeted interventions aimed at improving outcomes for affected individuals.
As the global healthcare community continues to grapple with the long-term implications of COVID-19, ongoing research endeavors are paramount in unraveling the intricacies of post-infectious neuroinflammation and developing effective strategies for managing PASC and promoting neurological recovery.
The study findings were published in the peer-reviewed journal: Scientific Reports (Nature).
https://www.nature.com/articles/s41598-024-57561-6
For the latest
COVID-19 News, keep on logging to Thailand Medical News.