COVID-19 News: Weill Cornell Study Finds That SARS-CoV-2 Infects And Triggers Senescence Of Dopamine Neurons! Metformin Helps!
Nikhil Prasad Fact checked by:Thailand Medical News Team Jan 18, 2024 2 years, 3 weeks, 2 days, 12 hours, 1 minute ago
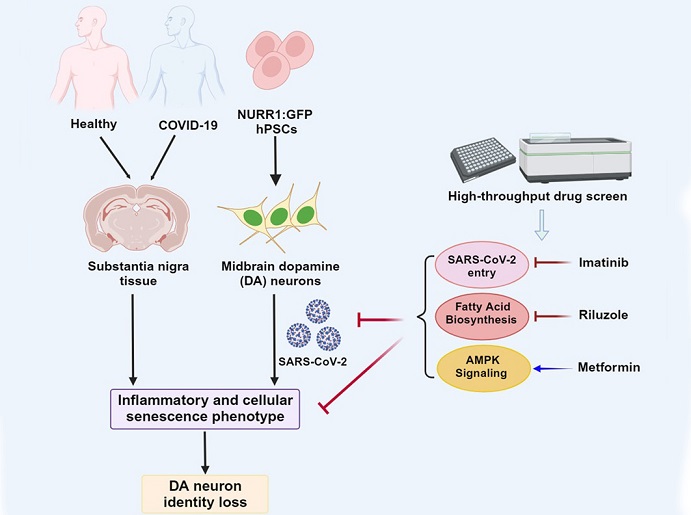
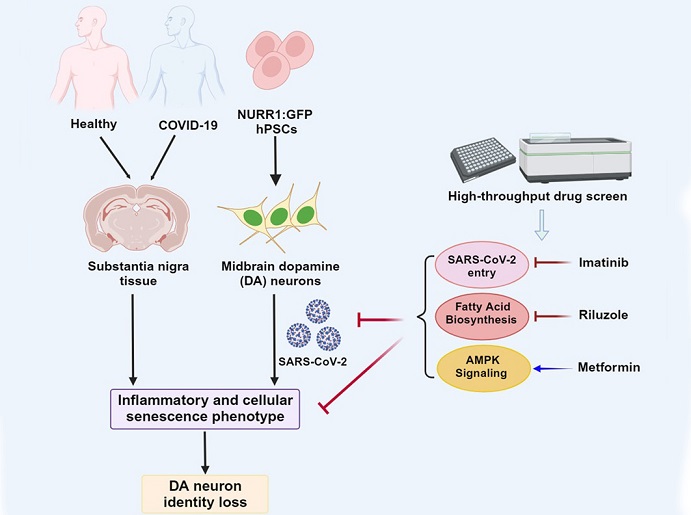
COVID-19 News: The global impact of the COVID-19 pandemic has led to an unprecedented surge in scientific research to understand the multifaceted ways in which the SARS-CoV-2 virus affects the human body. In a new study led by researchers at Weill Cornell Medicine-USA that also involved researchers from Memorial Sloan Kettering Cancer Center-USA and Columbia University Vagelos College of Physicians and Surgeons-USA, a startling revelation has emerged: SARS-CoV-2 has the ability to infect dopamine neurons in the brain, potentially offering key insights into long COVID symptoms such as brain fog and depression.
 SARS-CoV-2 Infects And Causes Senescence Of Dopamine Neurons That Can Result In Various Neuroligical Issues.
SARS-CoV-2 Infects And Causes Senescence Of Dopamine Neurons That Can Result In Various Neuroligical Issues.
Thailand Medical News in its previous
COVID-19 News coverages had also covered studies that showed the dopamine neurons were being infected by the SARS-CoV-2 virus and dopamine production was being hampered.
https://www.thailandmedical.news/news/breaking-covid-19-news-italian-study-shows-that-sars-cov-2-infects-dopaminergic-neurons-and-hampers-dopamine-production
https://www.thailandmedical.news/news/study-proposes-that-sars-cov-2-induced-neuroinflammation-causes-dopamine-dysfunction-and-transmission-imbalance,-contributing-to-long-covid
https://www.thailandmedical.news/news/breaking-coronavirus-news-saudi-arabia-study-shows-that-dopamine-receptors-might-be-targeted-by-sars-cov-2-coronavirus
The Discovery
The study initially sought to explore how various cell types respond to SARS-CoV-2 infection, examining lung cells, heart cells, pancreatic beta cells, and more.
However, the unexpected twist came when the researchers discovered a unique pathway exclusive to dopamine neurons. Approximately 5% of these neurons were found to be susceptible to SARS-CoV-2 infection, leading to a state of senescence - a condition where cells lose their ability to grow and divide. This senescence of dopamine neurons results in inflammation, offering a potential link to neurological symptoms associated with long COVID.
Key Findings
-Selective Vulnerability of Dopamine Neurons: The research unveiled the susceptibility of dopamine neurons to SARS-CoV-2 infection. While the infection rate in these neurons is not as high as in the virus's main target, lung cells, even a small population of infected dopamine neurons
could have severe consequences.
-Senescence Pathway Activation: The study utilized human stem cells to generate various cell types and found that only dopamine neurons activated the senescence pathway upon SARS-CoV-2 infection. This unexpected discovery indicates a potential mechanism through which the virus impacts the central nervous system.
-
Neurological Symptom Connection: Dopamine neurons play a crucial role in various brain functions, including pleasure, motivation, memory, sleep, and movement. The disruption caused by SARS-CoV-2 infection in these neurons may contribute to the development of neurological symptoms, possibly explaining the brain fog and depression reported by long COVID patients.
Diving Deeper into the Study's Methodology
The researchers leveraged human pluripotent stem cells (hPSCs) to generate midbrain dopamine (DA) neurons - a critical step in mirroring the human brain's complexity. Using a vesicular stomatitis ΔG-luciferase virus pseudotyped with the SARS-CoV-2 spike protein, they confirmed the susceptibility and permissiveness of DA neurons to the virus. Intriguingly, only a small percentage (approximately 5%) of DA neurons were infected, underlining the importance of this specific neuronal subtype.
The Senescence Pathway Unveiled
To unravel the impact of SARS-CoV-2 infection on DA neurons, the researchers performed gene expression analyses and observed the activation of the senescence pathway. This unique response was not observed in other neuronal cell types, such as cortical neurons. The senescence-associated secretory phenotype (SASP) was also identified, indicating the release of pro-inflammatory signals by the infected neurons.
Unveiling the Role of Specific Genes
The researchers identified specific genes associated with senescence, including CCL2, CCL20, CSF1, CXCL11, GDF15, IGF2R, IL1B, IL6ST, IQGAP1, and TNFRSF11B. The upregulation of these genes in SARS-CoV-2 infected DA neurons suggested a complex interplay between the virus and the cellular machinery, leading to inflammation and senescence.
Potential Implications for Parkinson's Disease
The study's unexpected findings open a new avenue for understanding the potential long-term consequences of SARS-CoV-2 infection. While the clinical relevance is still under exploration, the researchers suggest monitoring long COVID patients for an increased risk of developing symptoms related to Parkinson's disease. Given that DA neuron senescence is a hallmark of Parkinson's, this observation warrants further investigation through human population studies.
Exploring Genetic Factors
The researchers emphasize that exposure to COVID-19 does not uniformly impact individuals, and genetic factors may play a crucial role in determining susceptibility to neurological symptoms. Ongoing human population studies aim to unravel the complex interplay of disease severity, genetics, and the risk of neurological complications in COVID-19 patients.
Linking to Autopsy Samples
To further validate their findings, the researchers turned to autopsy samples from COVID-19 patients. Human substantia nigra samples from six COVID-19 patients and age-matched controls were analyzed. Remarkably, the transcriptional signatures observed in SARS-CoV-2 infected DA neurons in vitro mirrored those found in the substantia nigra of COVID-19 autopsy samples, strengthening the connection between viral infection and neuronal senescence.
The Intriguing Role of Alpha-Synuclein
The study delved deeper into the potential link between SARS-CoV-2 infection and Parkinson's disease by examining the impact on alpha-synuclein (α-Syn), a protein associated with PD. Notably, DA neurons with increased copy numbers of SNCA, a gene linked to familial PD, showed heightened susceptibility to SARS-CoV-2 infection. The subsequent increase in β-gal activity, lysosome accumulation, and total α-Syn expression underscored the intricate relationship between genetic factors and the virus's impact on neuronal health.
Identification of Potential Therapeutics
In a proactive move, the researchers screened a library of FDA-approved drugs to identify compounds that could mitigate SARS-CoV-2-induced senescence in DA neurons.
Through transcriptional profiling, they identified three existing drugs with promising results: riluzole (used to treat ALS or Lou Gehrig's disease), metformin (a diabetes medication), and imatinib (a cancer treatment).
These potential candidates were found to be good at reducing senescence in a dose-dependent manner without inducing cytotoxicity. These drugs demonstrated their efficacy by decreasing the percentage of β-gal+ cells and suppressing the expression of senescence-associated genes.
Further investigation into these drugs could lead to a preventive strategy against the virus's impact on the brain.
Unraveling the Mechanisms
To understand how these drugs exerted their protective effects, the researchers conducted further analyses. Riluzole, known for its use in treating ALS, demonstrated a downregulation of the fatty acid biosynthesis pathway. Metformin, a diabetes medication, upregulated the adenosine monophosphate-activated protein kinase (AMPK) pathway, which is involved in cellular energy homeostasis. Imatinib, a cancer treatment, exhibited a decrease in the expression of SASP-associated genes, highlighting its potential to modulate the inflammatory response induced by SARS-CoV-2 infection.
Implications for Future Research
As the scientific community grapples with the ever-evolving landscape of COVID-19 research, the study opens new doors for exploration. The unexpected link between SARS-CoV-2 and dopamine neurons not only provides a potential explanation for long COVID symptoms but also prompts a reevaluation of the neurological impact of viral infections.
Future research directions could include
-Population Studies: Extensive human population studies are warranted to understand the variability in susceptibility to SARS-CoV-2-induced neurological complications. Genetic factors, pre-existing conditions, and viral load dynamics may contribute to diverse outcomes.
-Therapeutic Development: The identified drugs - riluzole, metformin, and imatinib - present promising avenues for therapeutic development. Further preclinical and clinical studies are needed to validate their efficacy in preventing or mitigating neurological symptoms in COVID-19 patients.
-Longitudinal Monitoring: Given the potential link between SARS-CoV-2 infection and Parkinson's disease-related phenotypes, longitudinal monitoring of COVID-19 survivors becomes crucial. This will enable the identification of early signs of neurodegenerative disorders and the implementation of timely interventions.
Conclusion
In the relentless pursuit of understanding the intricate interactions between SARS-CoV-2 and the human body, the study findings emerge as a milestone. The discovery of SARS-CoV-2's impact on dopamine neurons and the subsequent activation of senescence pathways shed light on the complex interplay between viral infections and neurological health.
As the world grapples with the long-term consequences of the COVID-19 pandemic, this study not only unravels a novel aspect of the virus's pathology but also provides a foundation for future research and therapeutic development. The potential implications for long COVID, coupled with the unforeseen link to Parkinson's disease-related symptoms, underscore the urgency of comprehensive investigations into the neurological consequences of SARS-CoV-2 infection.
In the evolving landscape of COVID-19 research, each revelation contributes to a deeper understanding of the virus's impact, offering hope for more effective treatments and preventive strategies. The journey from laboratory discoveries to clinical applications is a complex one, but as the scientific community unites in the face of unprecedented challenges, the quest for knowledge remains a beacon of progress in our collective battle against the global pandemic.
The study findings were published in the peer reviewed journal: Cell Stem Cell.
https://www.cell.com/cell-stem-cell/fulltext/S1934-5909(23)00442-3
For the latest
COVID-19 News, keep on logging to Thailand Medical News.
Read Also:
https://www.thailandmedical.news/news/northwestern-study-shows-that-parkinson-s-is-caused-by-dysfunctional-dopaminergic-synapses-and-not-by-degeneration-of-dopaminergic-neurons