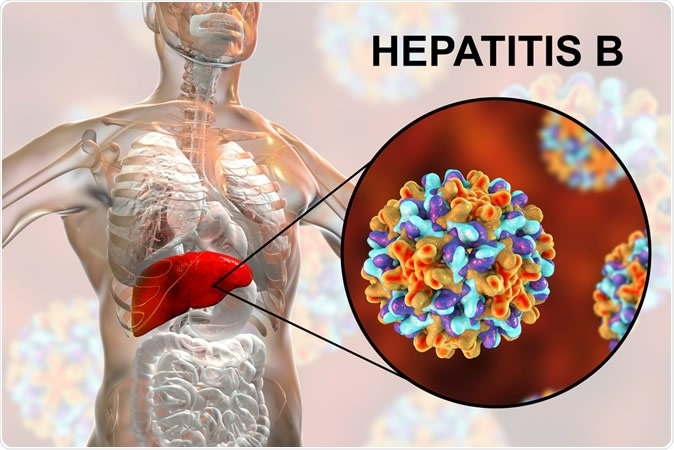
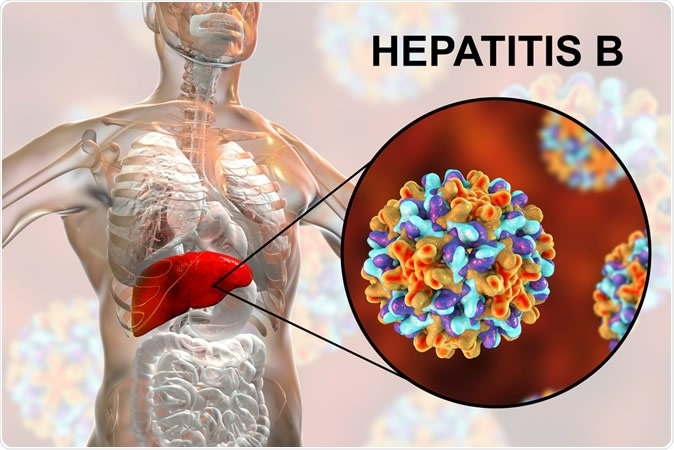
BREAKING! Hepatitis B: UAE COVID-19 Case Study Indicates That COVID-19 Could Induce Hepatitis B Virus Reactivation
Source: Hepatitis B and COVID-19 Jun 21, 2020 5 years, 8 months, 5 days, 19 hours, 19 minutes ago
Hepatitis B and COVID-19: Although the impaired liver function is prevalent in COVID-19, it is poorly understood. UAE researchers report the first case of hepatitis B virus (HBV) reactivation caused by COVID-19 in a young adult with altered mental status and severe transaminitis. The patient was asymptomatic, hypothermic, his skin was jaundiced with the icteric sclera, with very high levels of aspartate aminotransferase (AST; 4,933 U/L), alanine aminotransferase (ALT; 4,758 U/L), and total bilirubin (183.9 mmol/L) levels. It is warranted that patients with abnormal liver functions tend to have an increased risk of COVID-19. Thus, increased attention should be paid to the care of patients with abnormal liver functions, and testing for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) RNA is warranted in the COVID era.
The research findings are published in the journal : Cureus
https://www.cureus.com/articles/34714-covid-19-induced-hepatitis-b-virus-reactivation-a-novel-case-from-the-united-arab-emirates
It should be noted that this is not the first case of COVID19 reactivating dormant viruses in the body. There are cases of Epstein-Barr virus, Cytomegalovirus and even other dormant viral infections being reactivated in patients infected with COVID-19
According to the UAE researchers, a previously healthy 36-year-old man presented to the emergency department with an altered mental status. Two days prior to his hospitalization, the patient experienced intermittent vomiting, with two to three episodes that were reported to a local physician. As the patient progressed to unconsciousness, he was immediately transported to the emergency department. There was no history of fever, cough, shortness of breath, or sensitivity to light. Furthermore, there was no recent or remote history of travel, medication or herbal use, previous surgery, or sick contact with individuals with COVID-19. He did not have a history of consuming alcohol, drug abuse, or unprotected sexual intercourse. On admission, the patient was isolated and tested for COVID-19.
Interestingly, at the initial presentation, physical examination revealed hypothermia of 35.5°C, a pulse of 88/min, blood pressure of 136/78 mmHg, and respiratory rate of 20/min with a room air oxygen saturation of 98%. His skin was jaundiced with the icteric sclera. The liver edge was not palpable and did not reveal hepatomegaly. Chest and cardiovascular examinations were normal. His Glasgow Coma Scale (GCS) score was 7/15.
Briefly, laboratory findings were: AST 4,933 U/L (reference: <50 U/L), ALT 4,758 U/L (reference: <40 U/L), total bilirubin 183.9 mmol/L (reference: <21 mmol/L) with direct bilirubin 145 mmol/L (reference: <5 mmol/L), alkaline phosphatase (ALP) 212 U/L (reference: 40-129 U/L), and albumin 33 g/L (reference: 35-52 g/L) (see Table
1). In addition, his international normalized ratio (INR) was >10 (reference: 0.82-1.20). Except for ammonia 74 mmol/L (reference: 16-60 mmol/L), results for all other laboratory assessments such as complete blood count, total protein, and serum chemistry were unremarkable. Computerized tomography (CT) scan of the brain, chest X-ray, and Doppler ul
trasound of the liver were normal.
It was observed that the differential diagnoses for active viral hepatitis (A, C, and E), HIV, autoimmune hepatitis, Wilson’s disease, cytomegalovirus, and Epstein-Barr virus antibodies were negative. The patient tested negative for HIV, hepatitis A, hepatitis C, hepatitis E, cytomegalovirus, and Epstein-Barr virus antibodies. Additional liver workup revealed hepatitis B (HB) surface Ag-positivity, HB core Ab-positivity (IgM), HB envelop (HBe) Ag-negativity, and HBe Ab positivity, suggestive of reactivation of an HBV infection. His hepatitis B DNA viral load was 2,490 IU/mL (reference: <1000 IU/mL), confirming the diagnosis of an acute HBV infection. His COVID-19 polymerase chain reaction (PCR) test results were also positive.
The patient exhibited altered mental status and elevated enzymatic activities in the liver, admission into the ICU was initiated. The patient was started on lactulose via a nasogastric tube (NGT) and was administered cryoprecipitate on day 1. On day 2, entecavir (1 mg daily), vitamin K (10 mg daily), and intravenous thiamin (100 mg daily) administration were initiated. On day 3, his GCS improved to 11/15, with a gradual improvement in liver function parameters. Subsequently, he was shifted to the COVID-19 ward. On day 7, the patient regained complete consciousness (GCS: 15/15); his liver function parameters showed improvements with respect to transaminase and bilirubin levels. Multiple nasopharyngeal samples (3/4) for the SARS-CoV-2 PCR tested positive, but his chest X-ray remained normal. On day 16, his liver function parameters were in the cholestatic phase with decreasing transaminase levels. He tested negative for COVID-19 PCR twice, and the patient was eventually shifted to the general ward.
The UAE researchers reported a case of acute HBV reactivation in a COVID-19 patient with mental disturbances to the emergency department. The underlying pathogenesis of transient reactivation of HBV in COVID-19 remains unclear. This case illustrates the importance of an index of suspicion of acute liver injury in patients with COVID-19, as many present with varying degrees of liver test-result abnormalities. A recent meta-analysis of 35 studies identified the pooled prevalence of abnormal liver functions in COVID-19 patients was 19% (95% confidence interval: 9-32%) Hitherto, no cases of acute hepatitis and liver failure in COVID-19 patients have been reported. The patient tested positive for SARS-CoV-2 RNA in nasopharyngeal swab tests, even though he had no fever or respiratory symptoms. The researchers believe that this asymptomatic patient might have been capable of transmitting the virus as he was not isolated in the emergency department.
The UAE patient had an atypical presentation (altered mental status), which caused the reactivation of HBV, confirmed with strong immunological evidence. COVID-19-affected patients with digestive symptoms may require a longer time for the onset of their symptoms, delaying diagnosis considerably, as these symptoms are nonspecific. Given the high burden of liver diseases globally, it is believed that underlying liver conditions such as chronic HBV infection could be reactivated, contributing to elevated liver enzyme abnormalities in COVID-19. However, case studies of the interaction between pre-existing liver conditions and COVID-19 require meticulous evaluation. A recent review concluded that digestive symptoms and abnormal liver enzymes may play an important role in a large number of patients with COVID-19, particularly in those with atypical symptoms. Further studies are warranted to better understand the cause of liver injuries in patients with pre-existing liver diseases who have recently contracted COVID-19.
It was observed that elevated liver-related enzymes are reported in a substantial proportion of patients with COVID-19. The patient had elevated levels of liver aminotransferases, such as AST, ALT, and gamma-glutamyl transferase (GGT), during the subclinical phase. Contrastingly, Guan et al. identified an increased prevalence of abnormal liver aminotransferase levels, higher AST levels, and liver injury in severe cases of COVID-19 in a large cohort of 1099 patients. They observed elevated ALT (22%), AST (21%), and total bilirubin (10%) levels in patients affected with COVID-19. In the Fan et al. study, patients, specifically males, with abnormal liver test results, were more likely to have a moderate to a high degree of fever. In contrast, our patient was hypothermic at admission and showed very high levels of liver enzymes, total bilirubin, and ammonia and INR value.
The UAE researchers conclude that HBV reactivation was induced by COVID-19 in a young patient presenting with altered mental status and elevated liver enzyme levels. This indicates the liver might be a target organ for COVID-19 and the patients with abnormal liver functions tend to have a higher risk for SARS-CoV-2. Increased attention should be paid to care these patient groups, particularly, presentation of acute hepatitis warrants isolation and testing for SARS-CoV-2 RNA in the COVID era.
For more about
Hepatitis B and COVID-19, keep on logging to Thailand Medical News.