Nikhil Prasad Fact checked by:Thailand Medical News Team Oct 12, 2024 1 year, 3 months, 3 weeks, 1 day, 9 hours, 44 minutes ago
Medical News: In recent years, scientists have uncovered a surprising link between peroxisomes - small but crucial structures inside our cells - and inflammation in the brain. Peroxisomes play a key role in breaking down fats and controlling harmful molecules like reactive oxygen species (ROS), which can trigger inflammation. This
Medical News report delves into a new study exploring how these tiny organelles impact brain health, especially when things go wrong.
Researchers from the University of Maryland’s Shock, Trauma and Anesthesiology Research (STAR) Center, led by Dr. Chinmoy Sarkar and Dr. Marta Lipinski, have shed light on how peroxisomes influence neuroinflammation. The study findings could pave the way for new treatments for brain disorders, especially those involving inflammation.
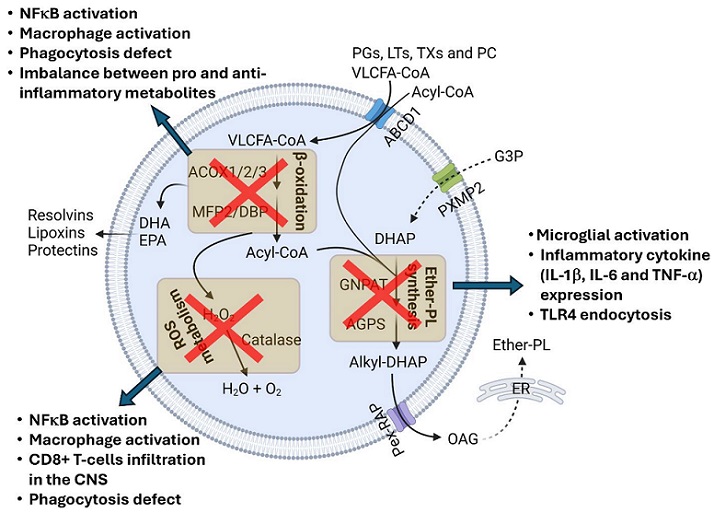
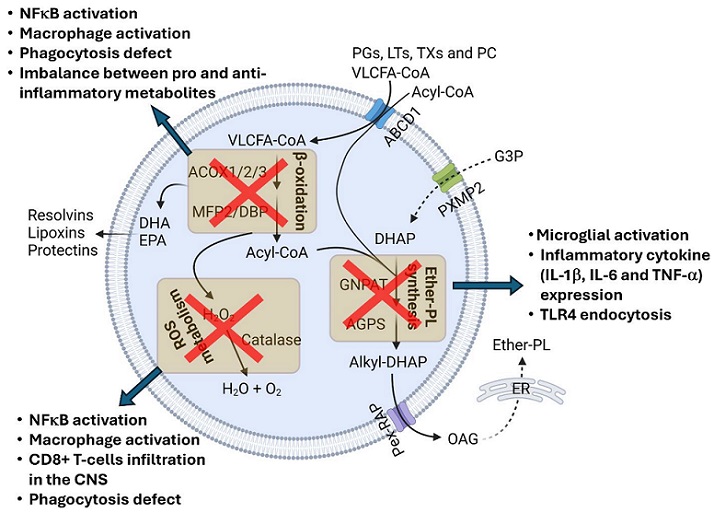 Peroxisomal impairment triggers inflammatory responses. An impairment to peroxisomal β-oxidation and ROS metabolism causes macrophage activation, the stimulation of the NFκB pathway, and phagocytosis defects. CD8+ T-cell infiltration in the CNS is associated with impaired peroxisomal ROS metabolism. Disruption in peroxisomal ether-PL synthesis activates the microglia, inducing inflammatory cytokine expression and TLR4 endocytosis
Peroxisomal impairment triggers inflammatory responses. An impairment to peroxisomal β-oxidation and ROS metabolism causes macrophage activation, the stimulation of the NFκB pathway, and phagocytosis defects. CD8+ T-cell infiltration in the CNS is associated with impaired peroxisomal ROS metabolism. Disruption in peroxisomal ether-PL synthesis activates the microglia, inducing inflammatory cytokine expression and TLR4 endocytosis
What are Peroxisomes?
Peroxisomes are tiny, single-membrane-bound organelles that help our cells maintain a balance in fat metabolism and oxidative stress. These processes are vital to keeping our cells healthy. Peroxisomes are best known for breaking down long-chain fatty acids and other harmful compounds. When they don't function properly, inflammation can occur, especially in the brain, where they are crucial in maintaining normal cellular functions.
Peroxisomes and Brain Inflammation
Neuroinflammation refers to inflammation within the brain or spinal cord. This happens when immune cells in the central nervous system, like microglia and astrocytes, become activated due to various triggers such as infections, stress, or injuries. Scientists have now discovered that peroxisomes play an important role in controlling neuroinflammation. When peroxisomes malfunction, harmful substances build up in the brain, contributing to inflammation and potentially leading to diseases such as Alzheimer's or multiple sclerosis.
According to the study, peroxisomes are involved in breaking down very-long-chain fatty acids (VLCFAs) through a process called β-oxidation. When this process is disturbed, VLCFAs accumulate, and inflammation follows. This process impacts immune cells and can even impair the brain's ability to protect itself from infections or injuries.
Key Functions of Peroxisomes
-Breaking Down Fatty Acids: One of the main roles of peroxisomes is to break down long-chain fatty acids through β-oxidation. This process helps prevent the build-up of these fats, which can be toxic in high amounts. VLCFAs are transported into the peroxisome, where they are broken down into smaller molecules that can be used for energy production in the mitocho
ndria.
-Maintaining Redox Balance: Peroxisomes contain enzymes that help manage oxidative stress. For example, the enzyme catalase breaks down hydrogen peroxide, a harmful byproduct, into water and oxygen. When peroxisomal functions are impaired, this balance is lost, leading to increased oxidative stress, which is a key driver of inflammation in the brain.
-Ether-Phospholipid Synthesis: Peroxisomes are also involved in the production of special lipids called ether-phospholipids (ether-PLs). These lipids are important for cell membranes and help protect the brain from oxidative stress. A disturbance in ether-PL production has been linked to neuroinflammatory diseases and brain aging.
The Link Between Peroxisomal Dysfunction and Neurodegenerative Diseases
Neuroinflammation is often linked to neurodegenerative diseases such as Alzheimer's disease, Parkinson’s disease, and multiple sclerosis. In these conditions, peroxisomes often malfunction, leading to the accumulation of VLCFAs and a decrease in essential lipids. This breakdown in peroxisomal function triggers a cascade of inflammatory responses, worsening disease symptoms. The study showed that disruptions in peroxisomal β-oxidation and ether-PL synthesis can result in neuroinflammatory conditions that contribute to the progression of these diseases.
Peroxisomal Disorders and Brain Inflammation
Certain genetic disorders, such as Zellweger syndrome and X-linked adrenoleukodystrophy (X-ALD), are caused by peroxisomal dysfunction and are often associated with severe neuroinflammation. In Zellweger syndrome, patients suffer from a range of symptoms, including severe brain inflammation, developmental delays, and early death. Similarly, in X-ALD, a deficiency in peroxisomal fatty acid transport leads to toxic buildup in the brain, causing severe inflammation and neurological damage.
The research from the University of Maryland highlights that the build-up of VLCFAs in patients with these disorders activates immune cells, such as microglia, which then produce inflammatory molecules like cytokines and chemokines. These substances further inflame brain tissues, leading to a vicious cycle of neuroinflammation.
The Role of Peroxisomes in Viral Infections and Immune Response
Peroxisomes are also emerging as key players in the body’s defense against viral infections. The study showed that peroxisomes can activate the body’s antiviral immune responses. For example, during a viral attack, peroxisomes can trigger the production of interferon, a protein that helps fight infections.
Interestingly, some viruses, such as the Zika virus, have found ways to evade this defense mechanism by damaging peroxisomes or disrupting their function. This discovery opens up new avenues for research into how boosting peroxisomal function could help improve immune responses and fight infections more effectively.
Potential Therapeutic Approaches
The findings from this study suggest that therapies aimed at improving peroxisomal function could offer new ways to treat neuroinflammatory diseases. By enhancing peroxisomal β-oxidation and ether-PL synthesis, it may be possible to reduce the harmful effects of VLCFAs and oxidative stress, helping to protect the brain from further inflammation and damage.
Researchers are exploring the possibility of developing drugs that target peroxisomes to boost their activity, particularly in aging brains where peroxisomal function tends to decline. Such treatments could be beneficial in managing neurodegenerative diseases by reducing inflammation and slowing down disease progression.
Conclusions
This research highlights the critical role peroxisomes play in maintaining brain health by regulating inflammation and protecting cells from damage. When peroxisomes malfunction, either due to genetic disorders or the aging process, the resulting buildup of harmful substances can trigger a cascade of neuroinflammation that contributes to neurodegenerative diseases.
Future research aimed at boosting peroxisomal function could lead to new therapies for treating brain inflammation and slowing the progression of conditions like Alzheimer's disease and multiple sclerosis. By focusing on improving the efficiency of these tiny cellular organelles, we may be able to find new ways to protect the brain and improve overall health.
The study findings were published in the peer-reviewed journal: Cells.
https://www.mdpi.com/2073-4409/13/19/1655
For the latest on Brain Inflammation, keep on logging to Thailand
Medical News.
Read Also:
https://www.thailandmedical.news/news/the-phytochemical-honokiol-from-the-magnolia-tree-combats-neuroinflammation-and-brain-aging
https://www.thailandmedical.news/news/indian-researchers-find-that-microrna-30b-5p-and-let-7a-5p-play-a-role-in-covid-19-related-brain-inflammation