University of Cambridge Researchers Discover That Hospitalized COVID-19 Patients Typically Exhibit Extreme Hypoaldosteronism
Source: COVID-19 Research - Hypoaldosteronism Mar 07, 2022 3 years, 11 months, 1 week, 1 day, 16 hours, 51 minutes ago
A new study by researchers from University of Cambridge and Cambridge University Hospitals NHS Foundation Trust has found that most hospitalized COVID-19 Patients typically exhibit extreme hypoaldosteronism, a condition characterized by the shortage (deficiency) or impaired function of a hormone called aldosterone.
Aldosterone is the main mineralocorticoid steroid hormone produced by the zona glomerulosa of the adrenal cortex in the adrenal gland. It is essential for sodium conservation in the kidney, salivary glands, sweat glands, and colon. It plays a central role in the homeostatic regulation of blood pressure, plasma sodium (Na+), and potassium (K+) levels. It does so primarily by acting on the mineralocorticoid receptors in the distal tubules and collecting ducts of the nephron. It influences the reabsorption of sodium and excretion of potassium (from and into the tubular fluids, respectively) of the kidney, thereby indirectly influencing water retention or loss, blood pressure and blood volume.
Importantly when dysregulated, aldosterone is pathogenic and contributes to the development and progression of cardiovascular and kidney disease. Aldosterone has exactly the opposite function of the atrial natriuretic hormone secreted by the heart.[
Past studies have reported conflicting findings regarding aldosterone levels in patients hospitalized with COVID-19.
The
COVID-19 Research study team hence used the gold-standard technique of liquid chromatography tandem mass-spectrometry (LCMSMS) to address this uncertainty.
The study involved patients admitted to Cambridge University Hospitals with COVID-19 between March 10, 2020 and May 13, 2021, and in whom a stored blood sample was available for analysis, were eligible for inclusion.
Aldosterone was measured by LCMSMS and by immunoassay; cortisol and renin were determined by immunoassay.
The study findings showed that aldosterone was below the limit of detection (<70 pmol/L) in 74 (58.7%) patients. Importantly, this finding was discordant with results obtained using a commonly employed clinical immunoassay (Liaison Diasorin®), which over-estimated aldosterone compared to the LCMSMS assay (intercept 14.1 [95% CI -34.4 to 54.1] + slope 3.16 [95% CI 2.09 to 4.15] pmol/L). The magnitude of this discrepancy did not clearly correlate with markers of kidney or liver function. Solvent extraction prior to immunoassay improved the agreement between methods (intercept -14.9 [95% CI -31.9 to -4.3] and slope 1.0 [95% CI 0.89 to 1.02] pmol/L) suggesting the presence of a water-soluble metabolite causing interference in the direct immunoassay.
The study team also replicated a previous finding that blood cortisol concentrations were often increased, with increased mortality in the group with serum cortisol levels >744 nmol/L (p=0.005).
Importantly, the study finding showed that when measured by LCMSMS, aldosterone was found to be profoundly low in a significant proportion of patients with COVID-19 at the time of hospital admission. This has likely not been detected previously due to high levels of interference with immunoassays in patients with COVID-19, and this merits further prospective investigation.
The study findings were published on a
preprint server and are currently being peer reviewed.
https://www.medrxiv.org/content/10.1101/2022.02.28.22271645v1
To date, the ongoing COVID-19 pandemic has caused almost 6 million deaths globally and excess deaths which are in the tens of millions, which has provoked intense research into the pathogenetic mechanism behind this disease.
The study findings indicate very low aldosterone levels in a subset of COVID-19 patients, thereby pointing to the involvement of renal hormones in the immunothrombotic and inflammatory phenomena typically seen in severe COVID-19.
The SARS-CoV-2 coronavirus, the pathogen responsible for COVID-19, binds to the angiotensin-converting enzyme 2 (ACE2) receptor to gain entry into the host cell. The ACE2 receptor is also a key component of the renin-angiotensin-aldosterone system (RAAS), which regulates renal and cardiovascular function in many ways.
Typically, ACE2 converts angiotensin II (AngII) to the anti-inflammatory and vasodilator antioxidant molecule Angiotensin 1-7 (Ang1-7), which allows for the inhibition of RAAS. Conversely, AngII is a powerful vasoconstrictor, pro-oxidant, and pro-inflammatory molecule that may also trigger fibrosis, aberrant coagulation, and immunothrombosis through its effect on the endothelium. This activity is mediated by endothelial production of tissue factor and plasminogen activator inhibitor 1.
Angiotensin II or angII also binds the adrenal angiotensin I receptor, which leads to the production of aldosterone, the major mineralocorticoid in the body. By binding with ACE2 and thus blocking AngII metabolism, SARS-CoV-2 can activate the RAAS and promote high aldosterone secretion. The excessive AngII activity may contribute to hypertension, thrombosis, inflammation, and lung fibrosis in COVID-19.
Previous studies have failed to demonstrate RAAS activation or low aldosterone levels; however, these studies often used non-specific methods that are very vulnerable to interference.
For this reason, the study team used mass spectrometry, as it is devoid of interference and provides more accurate estimates.
The study team had earlier witnessed several patients at their hospitals with low aldosterone, though this has not been reported as typical. In order to further examine this observation, the study team used liquid chromatography-tandem mass spectrometry (LC-MS) to estimate aldosterone levels in hospitalized COVID-19 patients.
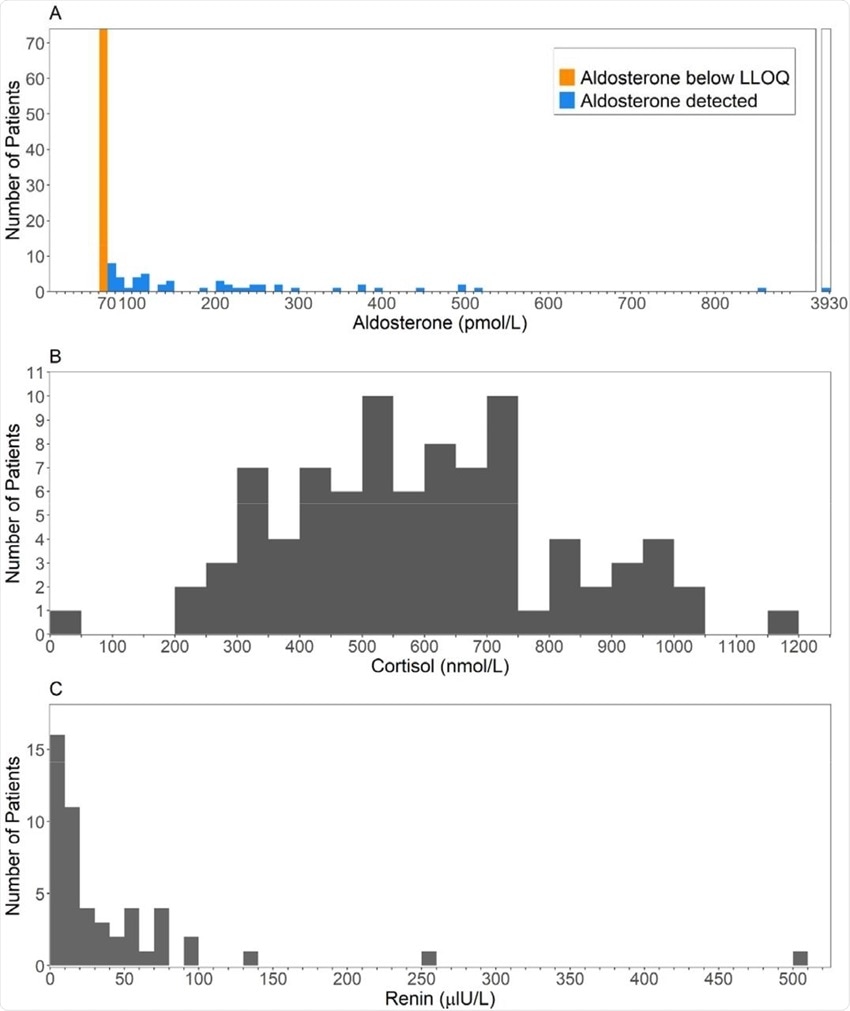 Histograms of the first available result (A) Aldosterone, measured using LCMSMS (B) Cortisol (C) Renin.
Histograms of the first available result (A) Aldosterone, measured using LCMSMS (B) Cortisol (C) Renin.
For the study, all patients had tested positive for SARS-CoV-2, all of which had a median age of 64 years. Of 134 patients with baseline aldosterone, cortisol, or renin levels within 72 hours of the first positive test for SARS-CoV-2, about 60% were male. About 11% of the patients were administered to the intensive care unit (ICU), with an in-hospital mortality rate of 13.4%.
The study findings showed that aldosterone concentrations were very low, with almost 60% having undetectable aldosterone levels below 70 pmol/L. Cortisol was higher than 744 nmol/L in 20.5% of patients, which represented the discriminant between survival and non-survival curves in earlier studies.
It was found that renin concentrations were also typically low, even though aldosterone levels were reduced, which would normally have increased renin levels.
Aldosterone levels were correlated with cortisol and renin concentrations; however, the lack of detectable aldosterone was not a marker for any clinical feature or outcome, survival, or renal function.
It was also found that high cortisol levels exceeding 744 nmol/L were linked to lower survival odds as compared to those with lower levels. That is, 44% of those in the former group died by 28 days as compared to 11% in the low cortisol group. Moreover, the high-cortisol cohort had a mean hospital stay of 19 days as compared to 11 days in the low-cortisol group.
Importantly a marked difference in survival was seen when cortisol levels exceeded 800 nmol/L in the high cortisol group.
Previous studies that used immunoassay methods to measure aldosterone levels failed to find any significant change in COVID-19 patients as compared to controls. The very different results with this study are attributed to the use of LC-MS. When the measurements were repeated by chemiluminescent immunoassay (CLIA), they found that CLIA (pmol/L) = 14.1 + 3.16 × LC-MS (pmol/L).
Hence, there is a major variation in the results obtained by these methods, which only increases as the mean measurements increase. These differences are not explained by altered renal or liver function.
Importantly, if the serum was subjected to solvent extraction, the results came into much closer agreement, where Extracted CLIA = -14.9 + 1.0 × LC-MS. This is explained by the presence of a water-soluble metabolite that interferes with the substance to be detected in the immunoassay.
Interestingly, the absence of clinical features of hypoaldosteronism has given rise to many hypotheses, including adequate mineralocorticoid activity to maintain the homeostasis of water and electrolytes. High cortisol levels may act at the mineralocorticoid receptor (MR), since the inactivating enzyme 11β-hydroxysteroid dehydrogenase type 2 (11β-HSD2) is saturated at these levels, thereby allowing glucocorticoid-MR crosstalk.
Thus, this could explain the lack of hypoaldosteronism clinically, but only in part because of the reduced correlation between cortisol and aldosterone levels in these patients. Aldosterone metabolites also do not appear to bind very strongly to the MR, thus ruling out their compensatory action.
Another possibility is that the activity of distal nephron epithelial sodium channels (EnaC) by AngII leads to increased reabsorption of sodium and an increase in blood volume, though potassium and hydrogen ions are excreted at a higher rate. This could initiate a vicious negative-feedback cycle for the RAAS, where renin and aldosterone levels fall further, even as AngII activity continues to be excessive due to the lack of ACE2 inhibition.
Significantly, the weak correlation between CLIA and LC-MS corroborates earlier studies while showing that COVID-19 exacerbates this issue. Solvent extraction probably eliminates a water-soluble metabolite that cross-reacts in the immunoassay. The prime candidate is the predominant aldosterone metabolite, aldosterone-18-glucuronide.
The study findings demonstrate that aldosterone cannot be accurately estimated in serum from patients with SARS-CoV-2 infection using direct competitive immunoassay. When measured using gold-standard LCMSMS, serum aldosterone is found to be remarkably low in most patients with COVID-19.”
The study findings also have implications about the reasons for increased cardiovascular and kidney issues in most COVID-19 patients.
Please help support this website by making a donation not only for the sustainability of the website but also for all our research and community initiatives. We are not funded by any entities and really need help. Your help not only saves lives directly but also indirectly.
https://www.thailandmedical.news/p/sponsorship
For the latest
COVID-19 research, keep on logging to Thailand Medical News.
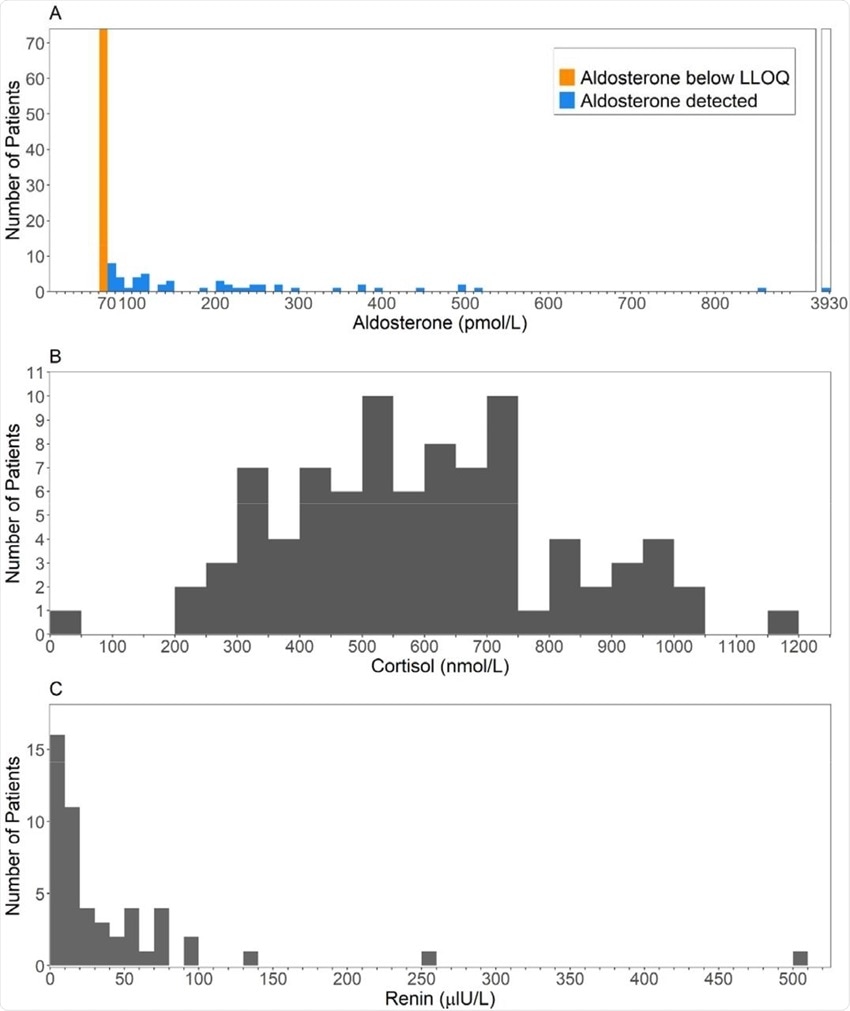 Histograms of the first available result (A) Aldosterone, measured using LCMSMS (B) Cortisol (C) Renin.
Histograms of the first available result (A) Aldosterone, measured using LCMSMS (B) Cortisol (C) Renin.