The Second Pandemic Concurrently-Long COVID. UCL Study Shockingly Identifies More Than 200 Long COVID Symptoms Across 10 Organ Systems!
Source: Long COVID News Jul 15, 2021 4 years, 7 months, 3 weeks, 1 day, 5 hours, 1 minute ago
With official figures stating that more than 188 million individuals globally have been infected with the COVID-19 disease and majority deemed ‘recovered’ but the US CDC and WHO saying the figures could be far much more ie tenfold, one cannot but feel worried about the impact of long term medical conditions from
Long COVID and how it is going to bring about the eventual collapse health care systems worldwide.
In a new study with startling findings, researchers from University College London-UK (UCL) and Presbyterian Hospital / Weill Cornell Medicine, New York City-USA and Oregon Health and Science University-USA have alarmingly found that the SARS-CoV-2 coronavirus and its variants are able to generate long term health conditions collectively known as Long COVID with can manifest more than 200 symptoms across ten organ systems!
A majority of patients with COVID-19 experience prolonged symptoms, known as Long COVID. Few systematic studies have investigated this population, particularly in outpatient settings. Thus, relatively little is known about symptom makeup and severity, expected clinical course, impact on daily functioning, and return to baseline health.
The study team conducted an online survey of individual with suspected and confirmed COVID-19, distributed via COVID-19 support groups (e.g. Body Politic, Long COVID Support Group, Long Haul COVID Fighters) and social media (e.g. Twitter, Facebook). Data were collected from September 6, 2020 to November 25, 2020.
The team analyzed responses from 3762 participants with confirmed (diagnostic/antibody positive; 1020) or suspected (diagnostic/antibody negative or untested; 2742) COVID-19, from 56 countries, with illness lasting over 28 days and onset prior to June 2020.
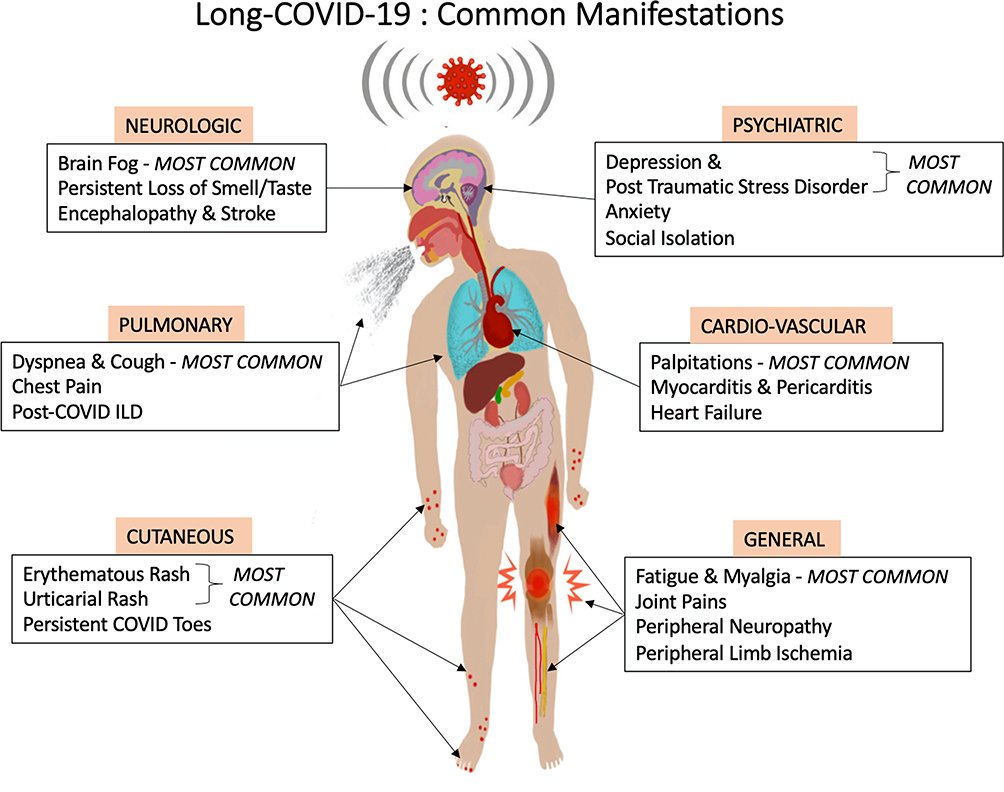
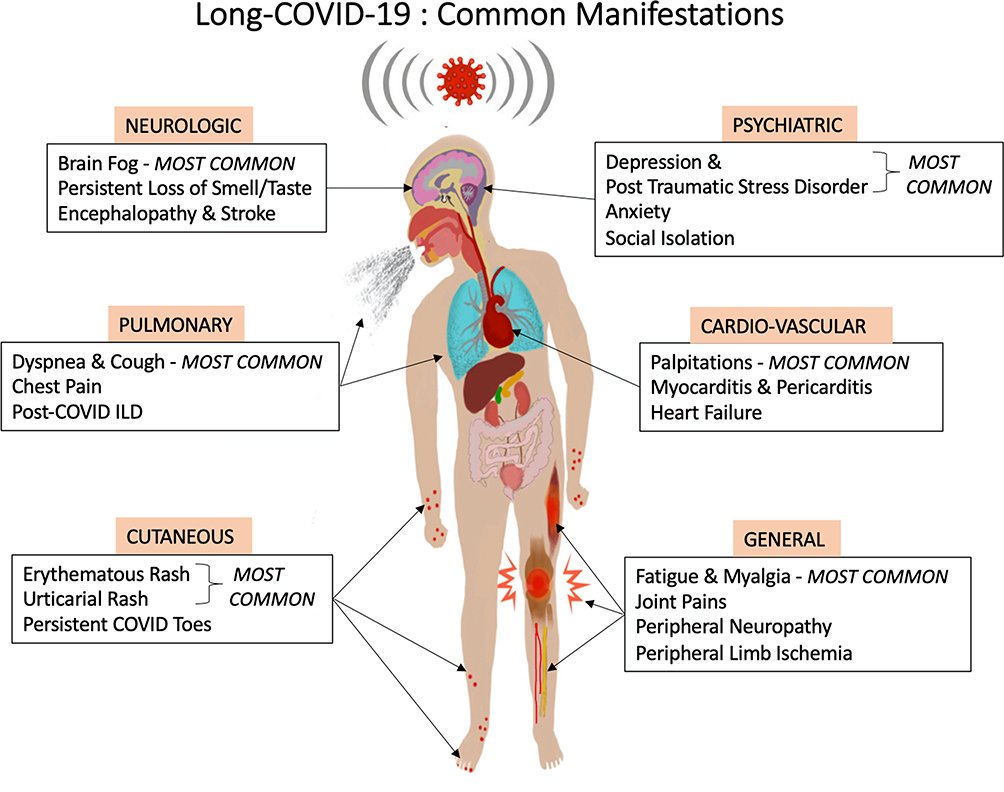
Shockingly the study team identified the prevalence of 203 symptoms in 10 organ systems and traced 66 symptoms over seven months.
The team measured the impact on life, work, and return to baseline health.
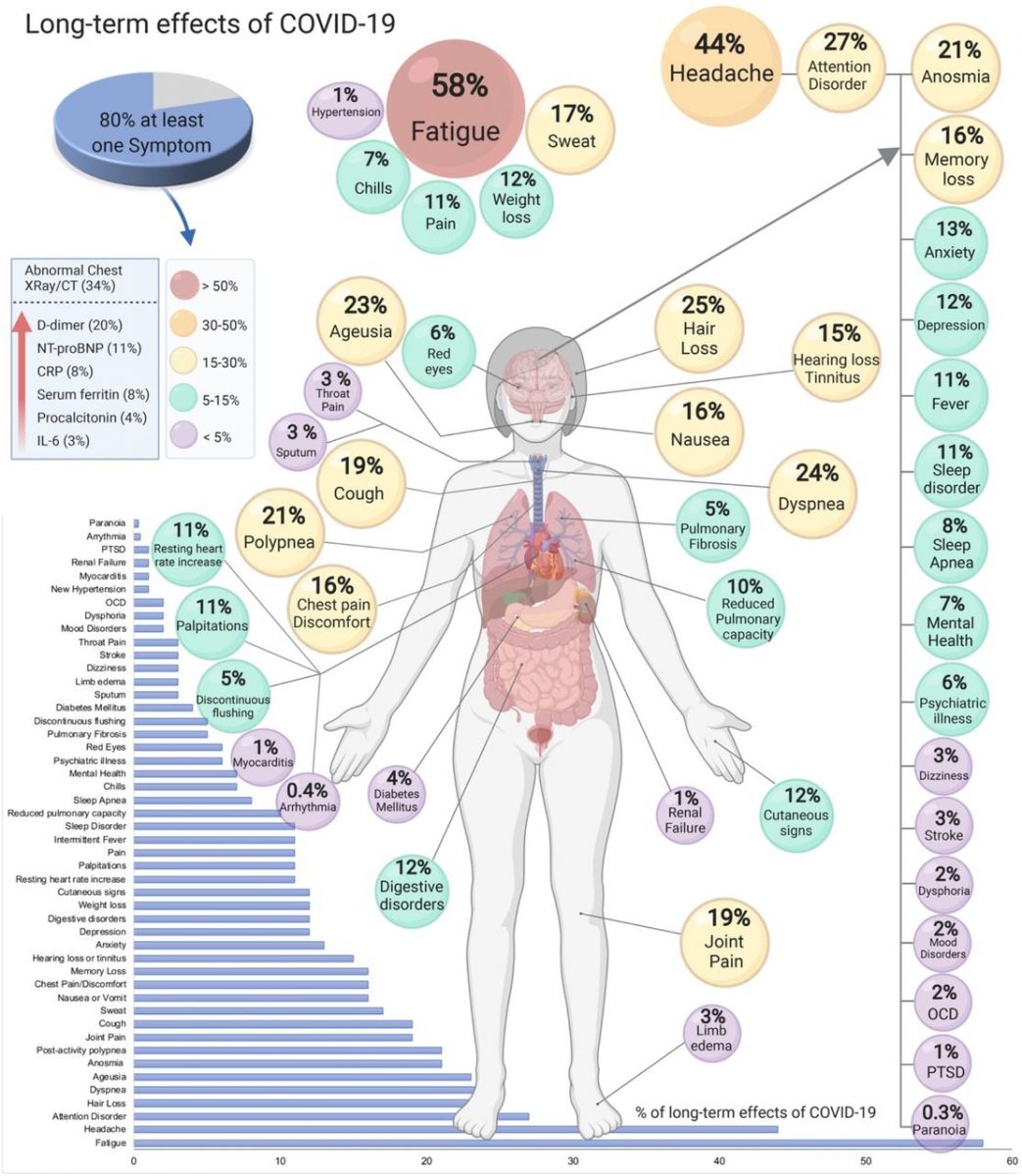
The study found that for the majority of respondents (>91%), the time to recovery exceeded 35 weeks. During their illness, participants experienced an average of 55.9+/- 25.5 (mean+/-STD) symptoms, across an average of 9.1 organ systems.
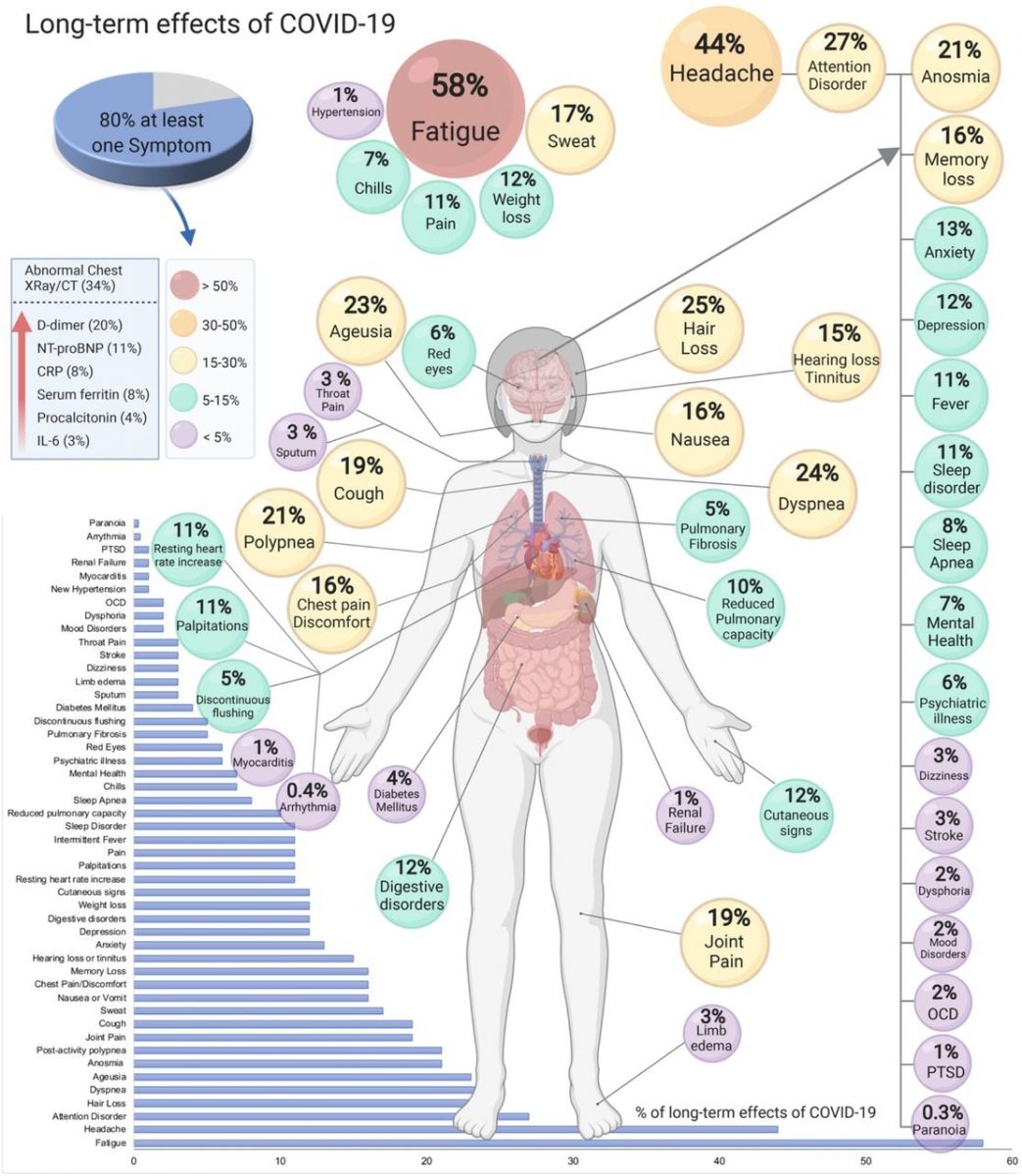
The most frequent symptoms after month 6 were fatigue, post-exertional malaise, and cognitive dysfunction. Symptoms varied in their prevalence over time, and the team identified three symptom clusters, each with a characteristic temporal profile. 85.9% of participants (95% CI, 84.8% to 87.0%) experienced relapses, primarily triggered by exercise, physical or mental activity, and stress. 86.7% (85.6% to 92.5%) of unrecovered respondents were experiencing fatigue at the time of survey, compared to 44.7% (38.5% to 50.5%) of recovered respondents. 1700 respondents (45.2%) required a reduced work schedule compared to pre-illness, and an additional 839 (22.3%) were not working at the time of survey due to illness. Cognitive dysfunction or memory issues were common across all age groups (~88%). Except for loss of smell and taste, the prevalence and trajectory of all symptoms were similar between groups with confirmed and suspected COVID-19.
‘Recovered’ patients with Long COVID reported prolonged, multisystem involvement and significant disability. By seven months, many patients have not
yet recovered (mainly from systemic and neurological/cognitive symptoms), have not returned to previous levels of work, and continue to experience significant symptom burden.
The study findings were published in the peer reviewed journal: Lancet’s EClinicalMedicine.
https://www.thelancet.com/journals/eclinm/article/PIIS2589-5370(21)00299-6/fulltext
This can be considered the largest study of ‘long-haulers’ to date led by scientists and a patient-led research collaborative in which patients who experience long COVID have reported more than 200 symptoms across 10 organ systems,
Scientists and ‘patient researchers’ who connected through the Body Politic online COVID-19 support group created a web-based survey designed to characterize the symptom profile and time course in patients with confirmed or suspected long COVID, along with the impact on daily life, work, and return to health.
Along with responses from 3,762 eligible participants from 56 countries, the study team identified a total of 203 symptoms in 10 organ systems; of these, 66 symptoms were tracked for seven months. The most common symptoms were fatigue, post-exertional malaise (the worsening of symptoms after physical or mental exertion), and cognitive dysfunction, often called brain fog.
Interestingly of the diverse range of symptoms, some included: visual hallucinations, tremors, itchy skin, changes to the menstrual cycle, sexual dysfunction, heart palpitations, bladder control issues, shingles, memory loss, blurred vision, diarrhea, and tinnitus.
The study team, who have all had or continue to have long COVID, are now calling for clinical guidelines on assessing long COVID to be significantly widened beyond currently advised cardiovascular and respiratory function tests to include neuropsychiatric, neurological, and activity intolerance symptoms.
Moreover, with large numbers of long haulers “suffering in silence,” the study team advocates that a national screening program, accessible to anyone who thinks they have long COVID, should be undertaken.
Considering the heterogeneous (diverse) make-up of symptoms that affect multiple organ systems, it is only by detecting the root cause that patients will receive the correct treatment.
Senior author Dr Athena Akrami (neuroscientist at the Sainsbury Wellcome Centre at UCL) explained, “While there has been a lot of public discussion around long COVID, there are few systematic studies investigating this population; hence relatively little is known about its range of symptoms, and their progression over time, the severity, and expected clinical course (longevity), its impact on daily functioning, and expected return to baseline health. In this unique approach, we have gone directly to ‘long haulers’ around the world in order to establish a foundation of evidence for medical investigation, improvement of care, and advocacy for the long COVID population. This is the most comprehensive characterization of long COVID symptoms, so far.”
The questionnaire was open to those aged 18 or over who had experienced symptoms consistent with COVID-19, including those with and without positive SARS-CoV-2 test. It consisted of 257 questions.
To characterize long COVID symptoms over an extended duration, analysis of survey data was limited to respondents with illnesses lasting longer than 28 days and whose onset of symptoms occurred between December 2019 and May 2020, allowing analysis of symptoms from week one to month seven.
Although the study did not estimate how common long COVID is overall, other studies have estimated that one in seven people have some symptoms 12 weeks after a positive test result (from the Office for National Statistics), or almost 30% of people 12 weeks after symptomatic disease (from Imperial College London’s REACT study).
Significantly in this long COVID cohort, the probability of symptoms lasting beyond 35 weeks (eight months) was 91.8%. Of the 3,762 respondents, 3,608 (96%) reported symptoms beyond 90 days, 2,454 (65%) experienced symptoms for at least 180 days (six months) and only 233 had recovered.
It was found that in those who recovered in less than 90 days, the average number of symptoms (11.4 out of 66 symptoms that were measured over time) peaked at week two, and for those who did not recover in 90 days, the average number of symptoms (17.2) peaked at month two. Respondents with symptoms over six months experienced an average of 13.8 symptoms in month seven.
During their illness, participants experienced an average of 55.9 symptoms (out of the longer list of 203 measured in the study), across an average of 9.1 organ systems.
Alarmingly 89.1% of participants experienced relapses, with exercise, physical or mental activity, and stress as the main triggers. 45.2% reported requiring a reduced work schedule compared to pre-illness and 22.3% were not working at all at the time of the survey.
The study team commented, “For the first time this study shines a light on the vast spectrum of symptoms, particularly neurological, prevalent and persistent in patients with long COVID. Memory and cognitive dysfunction, experienced by over 85% of respondents, were the most pervasive and persisting neurologic symptoms, equally common across all ages, and with substantial impact on work.”
They added, “Headaches, insomnia, vertigo, neuralgia, neuropsychiatric changes, tremors, sensitivity to noise and light, hallucinations (olfactory and other), tinnitus, and other sensorimotor symptoms were also all common, and may point to larger neurological issues involving both the central and peripheral nervous system. Along with the well-documented respiratory and cardiovascular symptoms, there is now a clear need to widen medical guidelines to assess a far wider range of symptoms when diagnosing long COVID. Furthermore, there are likely to be tens of thousands of long COVID patients suffering in silence, unsure that their symptoms are connected to COVID-19. Building on the network of long COVID clinics, which take GP referrals, we now believe a national program could be rolled out into communities able to screen, diagnose and treat all those suspected of have long COVID symptoms.”
The study team’s future work will focus on emerging topics in long COVID: mental health outcomes, diagnostic and antibody testing, symptom clustering, and socioeconomic impact from the illness.
The study authors did highlight several limitations to this study. First, the retrospective nature of the study exposes the possibility of recall bias. Second, as the survey was distributed in online support groups, there exists a sampling bias toward long COVID patients who joined support groups and were active participants of the groups at the time the survey was published. Additionally, despite eight translations and inclusive outreach efforts, the demographics were strongly skewed towards English speaking (91.9%), white (85.3%) respondents.
Summary Of Symptom Prevalence In Long COVID:
- The top three symptoms were: Fatigue 98.3%, post-exertional malaise (PEM) 89.0%, and brain fog and cognitive dysfunction in 85.1% (3,203) of respondents.
- The top three most debilitating symptoms listed by patients were: fatigue (2,652 patients), breathing issues (2,242), and cognitive dysfunction (1,274).
- Symptoms remaining at six months: A total of 2,454 (65.2%) respondents were experiencing symptoms for at least six months. Over 50% experienced the following symptoms: fatigue (80%) post-exertional malaise (73.3%), cognitive dysfunction (58.4%), sensorimotor symptoms (55.7%), headaches (53.6%), and memory issues (51%). In addition, between 30%-50% of respondents were experiencing the following symptoms after six months of symptoms: insomnia, heart palpitations, muscle aches, shortness of breath, dizziness and balance issues, sleep and language issues, joint pain, tachycardia, and other sleep issues.
-
- The 10 Organ systems affected:
- Systemic: fatigue, temperature, weakness, post-exertional malaise;
- Neuropsychiatric (sub-categories): Cognitive Functioning, Memory, Speech and Language, Neurological Sensations, Sleep, Headaches, Emotion and Mood, Taste and Smell, Hallucinations;
- Cardiovascular: heart related,
- Dermatologic: skin related
- Gastrointestinal: bowel/appetite-related symptoms;
- Pulmonary and Respiratory: breathing related;
- Head, Ear, Eye, Nose, Throat (HEENT): both physical and sensory symptoms to HEET;
- Reproductive, Genitourinary, and Endocrine: symptoms related to menstruation, thirst and urinary function, and low and high blood sugar;
- Immunologic and Autoimmune: new and heightened immune responses;
- Musculoskeletal: chest tightness and aches and pain throughout the musculoskeletal system
Overall, these findings suggest that the morbidity of COVID-19 illness has been greatly overlooked. Patients experience multisystem symptoms for over seven months, resulting in significant impact to their lives and livelihoods.
For the latest on
Long COVID-19, keep on logging to Thailand Medical News.
We are in the midst of creating a new site dedicated to Long COVID which will be fully functional by the 10th of August 2021. https://www.longcovid.news/ Be part of our team by helping to make a donation to support our causes and to sustain all our websites and to help all our research initiatives. https://www.thailandmedical.news/p/sponsorship