University Of Texas Study Findings Validates That SARS-CoV-2 Spike Protein Causes Endothelial Vascular Dysfunction
Source: COVID-19 Research Oct 06, 2022 3 years, 4 months, 1 week, 3 days, 5 hours, 31 minutes ago
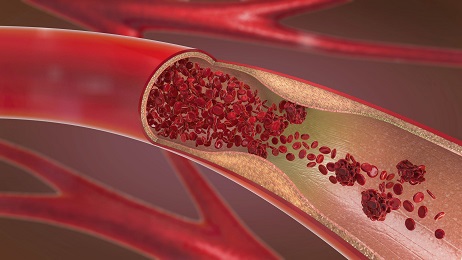
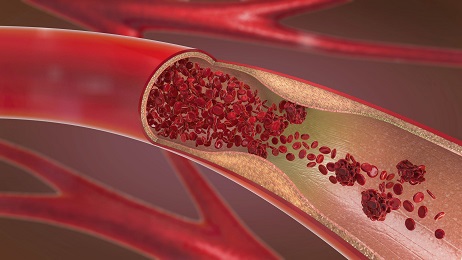
COVID-19 Research: The research findings of a new vitro study by researchers from the University of Texas-Austin-USA using three-dimensional engineered vascular networks has validated the previous claims that SARS-CoV-2 spike protein causes endothelial vascular dysfunction. The study findings not only have various implications on Long COVID but also about the usage of prophylactics and therapeutics that use these spike proteins to induce production of antibodies.
The study findings also showed that the usage of the glucocorticoid drug called Dexamethasone could help to prevent some of the vascular damage caused by the SARS-CoV-2 spike protein.
The study team said that as a result of the new daily discoveries about the long-term impacts of COVID-19 there is a clear need to develop
in vitro models that can be used to better understand the pathogenicity and impact of COVID-19.
The study team demonstrated the utility of developing a model of endothelial dysfunction that utilizes induced pluripotent stem cell-derived endothelial progenitors encapsulated in collagen hydrogels to study the effects of COVID-19 on the endothelium.
The
COVID-19 Research team found that treating these cell-laden hydrogels with SARS-CoV-2 spike protein resulted in a significant decrease in the number of vessel-forming cells as well as vessel network connectivity.
Interestingly, following treatment with the anti-inflammatory drug dexamethasone, the study team were able to prevent SARS-CoV-2 spike protein-induced endothelial dysfunction.
The study findings also confirmed the release of inflammatory cytokines associated with the COVID-19 cytokine storm.
The study findings demonstrated that even in the absence of immune cells, the study team was able to use the novel 3D
in vitro model for angiogenesis to reproduce COVID-19 induced endothelial dysfunction seen in clinical settings.
The study findings were published on a preprint server and are currently being peer reviewed.
https://www.biorxiv.org/content/10.1101/2022.10.01.510442v1
This is the first study to utilize a three-dimensional (3D)
in vitro tissue model to assess the effects of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) on the vascular endothelial cells.
Typically, in vitro models are required to improve understanding of coronavirus disease 2019 (COVID-19) pathogenicity.
In the past, in vitro, two-dimensional (2D) tissue models to study SARS-CoV-2 infection impacts on the endothelium have been developed with reduced cell adhesion molecule expression, endothelial barrier disruption, and enhanced inflammatory cytokine secretion in endothelial cells. However, due to the inability to simulate vascular networks, 2D models cannot model in vivo conditions as precisely as 3D models.
The study team previously used human-induced pluripotent stem cells (hiPSCs) that were differentiated into endothelial progenitors (EPs
) and encapsulated within collagen hydrogel structures to assess angiogenesis.
However, in the present study, the study team extended their previous analysis by creating a 3D model to study vascular network disruption in COVID-19.
In this study, hiPSCs derived from human dermal foreskin fibroblasts (DF19-19-9-11T) were cultured and differentiated into hiPSC-EPs. Subsequently, the cluster of differentiation (CD)34+ hiPSC-EPs were isolated by FACS (fluorescence-activated cell sorting) analysis and the CD34+ hiPSC-EP cells were encapsulated into a collagen hydrogel structure.
Next, the encapsulated hydrogels were cultured for a week to form capillary networks. After five days of encapsulation, the CD34+-hiPSC-EP-laden collagen hydrogels were SARS-CoV-2 spike (S) protein (CSP)-treated to simulate SARS-CoV-2 infections.
The study team next performed cytokine release assays to measure inflammatory cytokine expression after CSP treatment. The vessel-like networks generated within CD34+ iPSC-EP-laden collagen hydrogels were visualized by immunocytochemistry.
These cells were also treated with dexamethasone and visualized by confocal microscopy. The vessel length, vascular connectivity, and vessel lumen diameters were analyzed based on a previously developed computational pipeline.
SARS-CoV-2 mRNA or messenger ribonucleic acid from the hydrogels was subjected to qRT-PCR (quantitative reverse transcription–polymerase chain reaction) analysis to quantify mRNA expression based on the cycle threshold (Ct) values.
The study team also investigated whether CD34+-hiPSCs forming vascular networks within the collagen hydrogels expressed angiotensin-converting enzyme 2 (ACE2). In addition, the expression of several endothelial genes such as KDR (kinase insert domain receptor), CD31, CDH5 (cadherin 5), and CD34 were evaluated to track endothelial maturation over the one-week culture period and correlate the levels to ACE2 expression.
It was found that treatment with CSP significantly reduced the proportion of vessel-forming cells and vessel network connectivity in the hiPSCs-derived EPs encapsulated in collagen hydrogels.
Elevated inflammatory cytokine expression was observed in accordance with clinical findings, and 17 ng/mL dexamethasone treatment reduced vascular dysfunction in CSP-treated cells.
Importantly, even in the absence of immunological cells, the study team could use the 3D in vitro angiogenesis model to simulate the SARS-CoV-2 infection-induced dysfunction of endothelial cells representative of clinical COVID-19 presentations.
It was also found that following CSP treatment, the vascular network showed reduced density and more cells with an altered rounded morphology. CSP treatment (10 µg/mL) led to 22%, 33% and 29% reductions in vessel endpoints, vessel branch points, and vessel links, respectively. The corresponding reductions observed on using CSP in 100 µg/mL concentration were 17%, 24%, and 22%, respectively.
Also, vascular network connectivity loss was observed among CSP-treated collagen hydrogels with a 77% reduction in the proportion of cells that were a part of the largest vessel network.
It was also noted that when CSP was added on the first day, 19% and 31% reductions were observed in vessel branch points and volume fractions of collagen hydrogels comprising cells that form vessels, respectively.
The corresponding reductions observed when CSP was added on the fifth day were 59% and 66%, respectively, indicating higher CSP toxicity when added on the fifth day after vascular networks started to form.
The study findings also showed that ACE2 expression was highest on day 0 and reduced by 62% within a week post-CSP treatment.
The study team also observed 2.7-fold and 6.7-fold reductions in CD34 expression on the first and fifth days, respectively. Contrastingly, CD31 expression increased by two-fold, four-fold, and seven-fold on days 1, 5, and 7, respectively, and CDH5 expression increased by two-fold and three-fold on the fifth and seventh day, respectively.
The study findings showed that CSP treatment significantly increased interleukin-8 (IL-8) and chemokine C-X-C motif ligand 1 (CXCL1) release by two-fold and three-fold, respectively. Both cytokines are produced by endothelial cells and are upregulated in COVID-19.
The study findings indicated that CSP treatment created an inflammatory state comparable to the cytokine storm documented in severe COVID-19 cases.
The study team concluded that overall, the study findings showed successful reproduction of COVID-19-induced endothelial dysfunction observed in clinical settings using CSP-treated hiPSC-EP-laden collagen hydrogels. CSP treatment caused significant vascular disruption, concerning vascular network cells and vascular network connectivity, which was inhibited by dexamethasone.
The study findings validate that SARS-CoV-2 spike proteins causes endothelial dysfunction and significant vascular damage.
For the latest
COVID-19 Research, keep on logging to Thailand
Medical News.