SARS-CoV-2 Triggers Mast Cell Degranulation And Induces Respiratory Tract Epithelial Inflammation And Injury!
Nikhil Prasad Fact checked by:Thailand Medical News Team Mar 12, 2024 1 year, 11 months, 1 week, 2 days, 20 hours, 35 minutes ago
COVID-19 News: The COVID-19 pandemic caused by SARS-CoV-2 has posed a significant threat to global public health. A crucial pathological aspect of COVID-19 is the induction of hyper-inflammatory responses, leading to uncontrolled production of inflammatory cytokines and chemokines, resulting in multi-organ failure, particularly in the elderly and individuals with underlying health conditions. While systemic inflammation is recognized as the primary pathophysiological factor for COVID-19 complications, the specific mechanisms triggering inflammation remain incompletely understood.
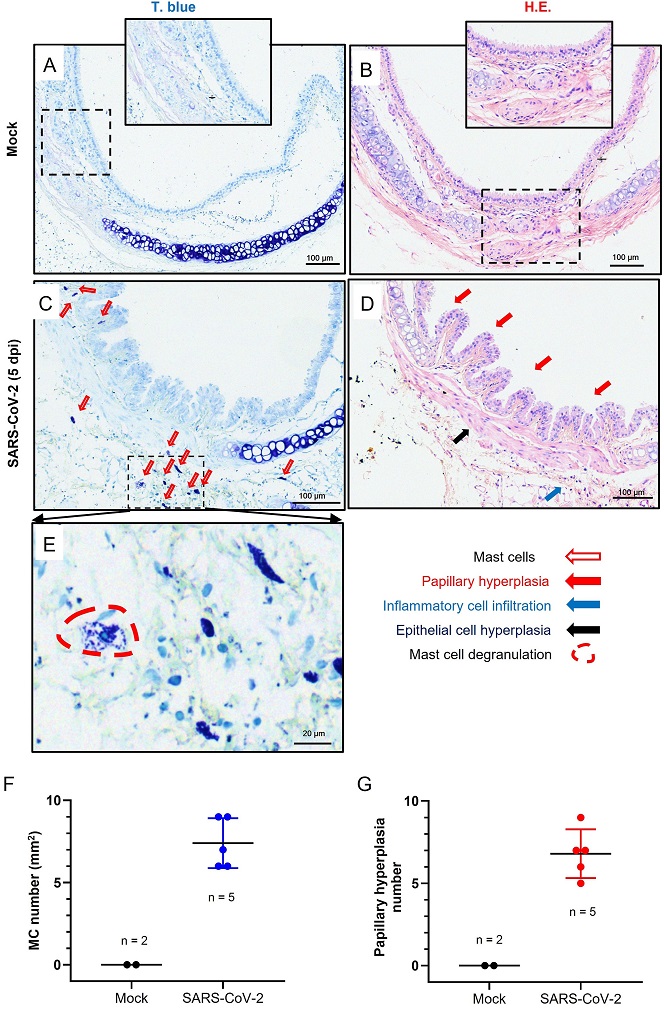
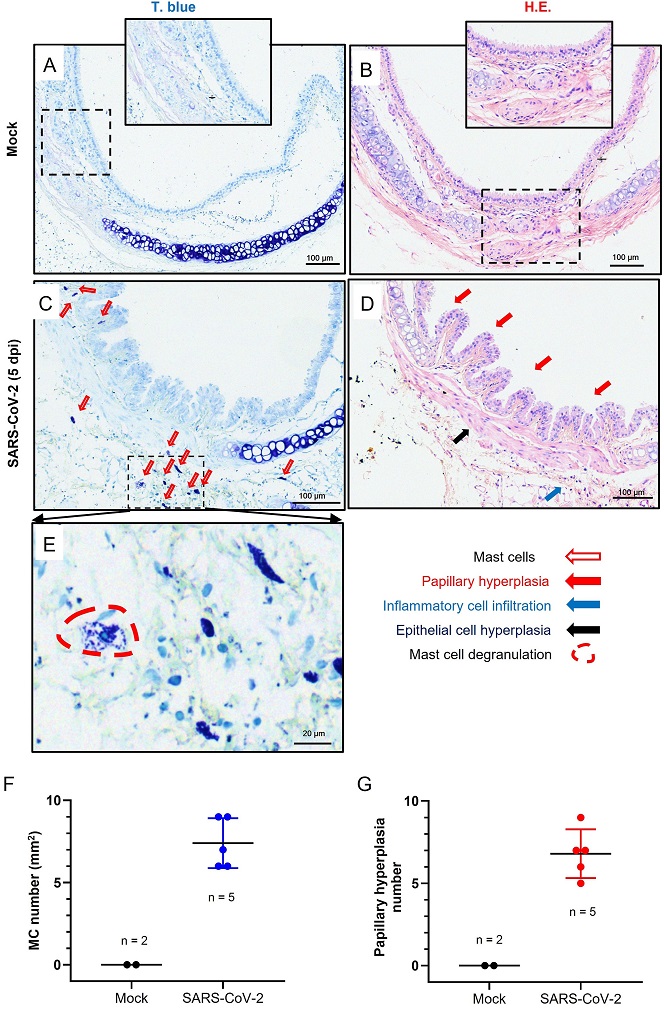 SARS-CoV-2 induces MC degranulation and trachea lesions in hACE2-humanized mice. The mice of C57BL/6N-ACE2em2(hACE2-WPRE, pgk-puro)/CCLA were intratracheally inoculated with SARS-CoV-2 (strain 107) at a dose of 5 × 106 TCID50. At day 5 post-infection, mice were anaesthetized and the trachea tissue were harvested for histological analysis. Toluidine blue (T. blue) staining was used to observe MCs and degranulation (A, C, E). Hematoxylin and Eosin (H.E.) staining was used to observe trachea injury (B, D). The PBS was used as the mock infection (A, B). (F–G) The counts of MC and papillary hyperplasia in trachea section were summarized. Scale bar: 100 or 20 μm. The number (n) of mouse used in tests was noted.
SARS-CoV-2 induces MC degranulation and trachea lesions in hACE2-humanized mice. The mice of C57BL/6N-ACE2em2(hACE2-WPRE, pgk-puro)/CCLA were intratracheally inoculated with SARS-CoV-2 (strain 107) at a dose of 5 × 106 TCID50. At day 5 post-infection, mice were anaesthetized and the trachea tissue were harvested for histological analysis. Toluidine blue (T. blue) staining was used to observe MCs and degranulation (A, C, E). Hematoxylin and Eosin (H.E.) staining was used to observe trachea injury (B, D). The PBS was used as the mock infection (A, B). (F–G) The counts of MC and papillary hyperplasia in trachea section were summarized. Scale bar: 100 or 20 μm. The number (n) of mouse used in tests was noted.
Research has shown that SARS-CoV-2 is primarily transmitted through the inhalation of respiratory droplets, affecting the nasal cavities, trachea, and large and small airways. The expression of the viral receptor ACE2 is heightened in these areas, making them susceptible to infection, especially in the elderly, smokers, and those with chronic lung diseases. The respiratory epithelium, comprising ciliated cells, secretory goblets, and basal cells, plays a crucial role in viral entry and spread. In this context, the study covered in this
COVID-19 News report by researchers from the Chinese Academy of Sciences, Guangzhou-China, University of Science and Technology of China, Hefei-China and Kunming Institute of Zoology, focuses on investigating the involvement of mast cells (MCs) and their degranulation in the development of inflammation in the tracheal-bronchial epithelium.
Mast Cells in SARS-CoV-2 Infection
MCs are tissue-resident cells strategically positioned at the host-environment interface, including the respiratory tract. Beyond their role in type I allergic reactions, MCs are increasingly recognized for their regulatory roles in various physiological processes. Studies have indicated the massive recruitment of MCs to the alveolar septa and pulmonary parenchyma in COVID-19 patients, with higher numbers correlating with increased disease severity. Our previous research demonstrated that SARS-CoV-2 infection led to MC accumulation and degranulation in humanized mice, particularly in the peri-bronchus and bronchioalveolar-duct junction.
MC Degranulation and Inflammatory Responses
r />
Our investigations revealed that MC degranulation induced by SARS-CoV-2 triggered inflammation in alveolar epithelial cells and capillary endothelial cells, resulting in lung injury. This degranulation was also observed in the trachea of infected mice, leading to papillary hyperplasia and evident tracheal lesions. Transcriptome analysis in bronchial epithelial cells exposed to MC degranulation highlighted significant alterations in cellular signaling, particularly upregulation of immune responses and inflammation.
To explore the therapeutic potential, we tested the administration of ebastine or loratadine, known MC stabilizers, in SARS-CoV-2-infected mice. Both compounds effectively suppressed the induction of inflammatory factors in bronchial epithelial cells and alleviated tracheal injury. These findings underscore the critical role of MC degranulation in SARS-CoV-2-induced hyper-inflammation and support the use of ebastine or loratadine to mitigate tissue damage caused by inflammation.
Mast Cell Degranulation and Respiratory Tract Injury
Our study sheds light on the mechanisms underlying SARS-CoV-2-induced hyper-inflammation, emphasizing the importance of various cell types and signaling pathways in this process. Infected epithelial cells initiate robust immune responses, releasing inflammatory cytokines that recruit and activate immune cells, contributing to systemic inflammation. Notably, we observed rapid MC degranulation in the lungs of SARS-CoV-2-infected mice and nonhuman primates, leading to lung inflammation and damage. The severity of disease in humans is associated with the activation of lung MCs.
The trachea and bronchus serve as the primary route for SARS-CoV-2 transmission through inhalation, and inflammation in these regions may facilitate viral invasion and spread. Our previous studies demonstrated the interaction between the spike protein and the ACE2 receptor, inducing MC degranulation. This study further investigates the role of MC degranulation in tracheal-bronchial inflammation, revealing its significance in promoting tissue lesions and subsequent complications.
Inflammatory Factors Induced by MC Granules
MC granules contain various mediators, including histamine, serotonin, heparin, cytokines, and enzymes like chymase and tryptase. We found that SARS-CoV-2-induced MC degranulation led to the release of histamine, chymase, and tryptase, which stimulated the expression of inflammatory factors in human respiratory epithelial cells. Notably, the treatment with ebastine or loratadine reduced the production of inflammatory factors, providing a potential avenue for therapeutic intervention.
Therapeutic Potential of Mast Cell Stabilizers
To further explore the therapeutic potential, we evaluated the impact of ebastine and loratadine on SARS-CoV-2-induced respiratory tract injury in mice. Administration of these compounds significantly reduced MC accumulation and degranulation, mitigating trachea lesions. This suggests that MC stabilizers may offer clinical benefits by suppressing hyper-inflammation and preventing tissue damage in COVID-19 patients.
Conclusion
In conclusion, our study provides valuable insights into the role of mast cell degranulation in SARS-CoV-2-induced respiratory inflammation and injury. The findings highlight the importance of targeting MC activation as a potential therapeutic strategy to mitigate the hyper-inflammatory response associated with COVID-19. The use of mast cell stabilizers such as ebastine and loratadine emerges as a promising approach to protect against tissue damage caused by hyper-inflammation in the respiratory tract. Further research and clinical trials are warranted to validate the efficacy and safety of these compounds in the context of COVID-19 management.
The study findings were published in the peer reviewed journal: Virologica Sinica.
https://www.sciencedirect.com/science/article/pii/S1995820X24000270
For the latest COVID-19 News, keep on logging to Thailand Medical News.