Nikhil Prasad Fact checked by:Thailand Medical News Team Jan 16, 2024 2 years, 1 month, 3 hours, 17 minutes ago
COVID-19 News: The global COVID-19 pandemic, spurred by the SARS-CoV-2 virus, has transcended the boundaries of respiratory distress, unraveling a spectrum of health issues that extend into the realm of bone health and musculoskeletal complications. In this
COVID-19 News report, we delve into the research efforts of the Indiana University School of Medicine in Indianapolis, USA, and Eastern Virginia Medical School in Norfolk, USA, shedding light on the intricate details of this novel facet of the pandemic.
 COVID-19 Can Lead To Bone Loss
Recent Findings and Clinical Evidence
COVID-19 Can Lead To Bone Loss
Recent Findings and Clinical Evidence
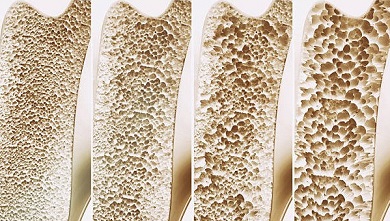
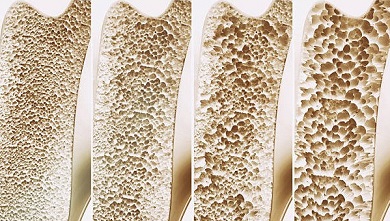
Emerging clinical evidence has highlighted a heightened risk of bone-related issues in COVID-19 patients, including vertebral fractures, hypocalcemia, vitamin D deficiencies, and reduced bone mineral density (BMD). Notably, lower BMD correlates with more severe SARS-CoV-2 infections, prompting a closer look at the underlying mechanisms. Preclinical models have mirrored these clinical findings, indicating increased osteoclastogenesis and bone loss, emphasizing the multifaceted impact of COVID-19 on the skeletal system.
Systemic Effects Beyond Pulmonary Issues
COVID-19's impact extends beyond the respiratory system, manifesting as joint pain (arthralgia), muscle pain (myalgia), and an increased risk of acute kidney injury (AKI). Disease severity in SARS-CoV-2 infection is influenced by factors such as obesity, age, and pre-existing conditions like diabetes. A subset of patients experiences a "cytokine storm," associated with severe multiorgan dysfunction, further complicating the clinical picture.
Post-acute sequelae of COVID-19 (PASC) present a syndrome with various manifestations, including kidney failure, inflammation markers, immune cell infiltration, and endothelial injury. The musculoskeletal system contributes with myalgia, joint pain, sarcopenia, and heterotopic ossification. Researchers and healthcare professionals are actively investigating the long-term and systemic effects of SARS-CoV-2 infection to understand comorbidities and treatment options for COVID-19 survivors.
Clinical Evidence of SARS-CoV-2 Infection-Related Bone Loss
Observations from the pandemic have emphasized alterations in mineral metabolism and bone turnover markers in COVID-19 patients. Hypocalcemia, commonly seen in other viral infections, is prevalent among COVID-19 patients, and early studies have linked it to a higher frequency of hospitalization.
Additionally, bone turnover markers like CTX and osteocalcin were lower in SARS-CoV-2-infected patients, indicating reduced bone turnover.
Vertebral fractures (VF), indicators of poor bone quality, were highly prevalent in COVID-19 patients. The severity of the disease, mortality, and the need for mechanical ventilation influenced outcomes. Larger studies revealed that VFs were not exclusive to COVID-19 patients, and mortality risk was significantly higher only in those with multiple fractures. Correlations between lower BMD and the severity of SARS-
CoV-2 infection were evident even in non-severe cases, indicating a broader impact on bone health.
In Vitro and Preclinical Insights
In vitro studies have played a pivotal role in understanding how SARS-CoV-2 directly affects bone marrow cells. Human monocytes expressing ACE2, the receptor used by the virus for cell entry, are potential targets for infection. Exposure to SARS coronavirus proteins increased osteoclastogenesis, suggesting a direct impact on bone-related cells.
Recent in vitro research on murine bone marrow cells exposed to the SARS-CoV-2 spike protein revealed potential infection of macrophages. Changes to the senescence-associated secretory phenotype (SASP) were observed, indicating alterations in cellular differentiation within the bone marrow. In preclinical models involving genetically modified mice expressing human ACE2 (hACE2) and hamster models, trabecular bone loss and increased osteoclastogenesis were observed, irrespective of disease severity.
Unveiling the Intricate Cellular Mechanisms
The intricate cellular mechanisms through which SARS-CoV-2 influences bone health encompass various aspects, underscoring the complexity of the relationship between the virus and the musculoskeletal system. From heightened inflammation and inflammasome activation to immune responses, hypoxia, and indirect effects on bone through muscle weakness and nutritional deficiencies, the multifaceted nature of these interactions demands further investigation.
-Inflammation - A Double-Edged Sword
Inflammation, a central mechanism in SARS-CoV-2 infection, plays a dual role in bone health. While inflammation is a crucial component of the immune response, chronic inflammation can have detrimental effects on tissues, including bone. The inflammatory response in COVID-19 leads to an increase in reactive oxidative species (ROS) and advanced glycation end-products (AGEs), potentially causing protein damage and crosslinks in bone, rendering it more brittle.
The activation of the receptor for AGEs (RAGE) in the inflammatory environment may contribute to increased osteoclastogenesis, further affecting bone turnover. The intricate interplay between inflammation and bone cells highlights the multifaceted nature of SARS-CoV-2's influence on bone health.
-NLRP3 Inflammasome - Orchestrating Bone Dynamics
The NLRP3 inflammasome, a molecular complex involved in regulating inflammatory responses, has implications for bone and joint diseases. Activation of the NLRP3 inflammasome has been linked to bone loss, with deficiencies being protective against bone loss in preclinical models. Research suggests that SARS-CoV-2 infection activates the NLRP3 inflammasome, providing a potential cellular mechanism for bone alterations. The interaction between the ACE2 receptor and the virus's spike protein triggers NLRP3 inflammasome activation in bone marrow cells, further supported by clinical evidence of elevated IL-1β and IL-18 in COVID-19 patients.
-Th17 Cells - Immune Response and Bone Regulation
T helper 17 cells (Th17) play a crucial role in immune responses and autoimmune disorders by producing IL-17. Th17 cells regulate osteoclastogenesis through the release of IL-17, influencing the fracture healing process. Increased Th17 activity observed in SARS-CoV-2 infection contributes to the "cytokine storm" associated with severe COVID-19. The dysregulation of inflammatory responses, reflected in decreased Th cells and Treg cells, suggests a potential imbalance impacting bone health. Th17 cells' ability to modulate osteoclastogenesis and influence bone cells underscores their significance in understanding the intricate connection between the immune response and bone dynamics during SARS-CoV-2 infection.
-Hypoxia - A Double-Edged Sword for Bone Loss
Hypoxia, characterized by low oxygen levels, has both detrimental and stimulatory effects on bone health. In vitro hypoxia conditions impair osteoblast proliferation but stimulate osteoclast formation and activity. SARS-CoV-2 infection induces hypoxia in patients, particularly those with severe disease, raising questions about its role in promoting osteoclastogenesis and impairing osteoblastogenesis, especially in the presence of obesity, a common comorbidity in severe cases.
-RANK/RANKL/OPG Signaling - Balancing Bone Remodeling
The intricate RANK/RANKL/OPG signaling pathway plays a crucial role in osteoclastogenesis, with RANKL inducing osteoclast differentiation and OPG serving as a decoy receptor to suppress it. Alterations in the RANKL/OPG ratio in COVID-19 patients, with conflicting results on OPG levels, indicate changes that may suggest increased osteoclast activity or a compensatory response to maintain bone homeostasis.
-Indirect Effects on Bone - Muscles, Nutritional Deficiencies, and Steroid Utilization
Systemic effects of SARS-CoV-2 extend to muscle weakness and mechanical unloading, indirectly affecting bone health.
Myalgia and muscle inflammation, observed in severe cases, contribute to muscle wasting and decreased strength, impacting bone mass. The breakdown of muscle tissue may adversely affect skeletal muscle mitochondria, influencing bone health acutely and chronically.
Nutritional deficiencies, particularly in vitamin D and trace elements like zinc and selenium, complicate the bone-health landscape. Low vitamin D levels in COVID-19 patients, with potential implications for immune regulation and inflammatory responses, are reported. However, the effects of supplementation on bone health in SARS-CoV-2-infected individuals require further exploration.
Corticosteroid usage, beneficial for managing severe COVID-19 cases, poses a potential risk to bone health. Glucocorticoids, in particular, have direct effects on bone, leading to reduced bone mineral density and alterations in osteoclast and osteoblast activity. The interplay between steroid utilization and the direct effects of SARS-CoV-2 infection on bone requires careful consideration in future investigations.
-Concurrent Conditions and Severity of COVID-19: The Role of Obesity and Diabetes, Acute Kidney Injury, and Chronic Kidney Disease
Concurrent conditions significantly influence the severity and outcomes of COVID-19, with obesity and diabetes being notable contributors. Both conditions are associated with increased inflammatory markers, potentially exacerbating the "cytokine storm" observed in severe SARS-CoV-2 infection. The inflammatory milieu, combined with altered immune responses, may contribute to increased osteoclast activity and bone resorption.
Acute kidney injury (AKI) and subsequent chronic kidney disease (CKD) add another layer to the bone-health interplay in the context of SARS-CoV-2 infection. AKI increases the risk of fractures, likely through disruptions in calcium and phosphorus homeostasis. CKD, characterized by mineral disorders and elevated levels of fibroblastic growth factor-23 (FGF-23), further complicates the bone-health landscape.
Future Directions and Conclusion
As researchers navigate the uncharted territory of COVID-19's impact on bone health, several questions remain unanswered. Future research endeavors should aim to identify specific patient populations at a higher risk of COVID-19-related fractures, unravel the intricate mechanisms behind bone loss, and explore therapeutic options to mitigate these effects.
Comparative studies on different SARS-CoV-2 variants and their unique impact on bone health are essential for a nuanced understanding. The lack of preclinical studies directly comparing the effects of different variants emphasizes the need for further investigations in this area.
In conclusion, the relationship between COVID-19 and bone health is a multifaceted puzzle that demands continued exploration. From clinical evidence highlighting altered mineral metabolism and increased fracture risk to in vitro and preclinical models providing insights into direct effects on bone cells, the intricate web of COVID-19's impact on bone health is slowly unraveling. A more comprehensive understanding will guide future preventive and therapeutic strategies, offering hope for mitigating the long-term musculoskeletal effects of the ongoing pandemic.
The study findings were published in the peer reviewed journal: Current Osteoporosis Reports (Springer Link).
https://link.springer.com/article/10.1007/s11914-023-00842-2
For the latest
COVID-19 News, keep on logging to Thailand Medical News.
Read Also:
https://www.thailandmedical.news/news/breaking-new-hong-kong-study-reveals-that-sars-cov-2-infections-also-causes-inflammatory-bone-loss-leading-to-long-covid-skeletal-health-issues
https://www.thailandmedical.news/news/covid-19-news-slovakian-study-shows-that-covid-19-pandemic-has-affected-the-bone-density-of-young-adults-possibly-due-to-lifestyle-changes
https://www.thailandmedical.news/news/covid-19-news-scientists-warns-of-the-impact-of-sars-cov-2-on-the-musculoskeletal-system-and-calls-for-more-research
https://www.thailandmedical.news/news/breaking-sars-cov-2-targets-endothelin-receptors,-causing-bone-and-cartilage-damage-and-joint-pains-endothelin-receptor-blocker-macitentan-helps
https://www.thailandmedical.news/news/brazilian-study-validates-that-covid-19-infections-also-affects-the-musculoskeletal-system
https://www.thailandmedical.news/news/southern-illinois-university-edwardsville-study-finds-that-most-exposed-to-sars-cov-2-will-develop-viral-arthropathy-besides-myalgia
https://www.thailandmedical.news/news/sars-cov-2-can-infect-bone-marrow-derived-macrophages-and-alter-the-expression-of-macrophage-chemotaxis-and-osteoclast-related-genes