Cerebral Microstructural Changes Linked to Cognitive, Olfactory, and Fatigue Symptoms in Post-COVID Condition
Nikhil Prasad Fact checked by:Thailand Medical News Team May 22, 2024 1 year, 8 months, 3 weeks, 4 days, 3 hours, 57 minutes ago
COVID-19 News: The COVID-19 pandemic, caused by the SARS-CoV-2 virus, has left an indelible mark on global health. Beyond the immediate respiratory implications, a significant number of individuals experience long-lasting effects collectively referred to as Post-COVID Condition (PCC). Characterized by a range of symptoms including cognitive deficits, olfactory dysfunction, and persistent fatigue, PCC affects a substantial proportion of COVID-19 survivors. Despite its prevalence, the pathophysiological mechanisms underlying these symptoms remain poorly understood, and biomarkers are scarce. This
COVID-19 News report explores the cerebral microstructural alterations in PCC and their association with cognitive impairment, olfactory dysfunction, and fatigue, using advanced magnetic resonance imaging (MRI) techniques in a study conducted by researchers from the University of Freiburg-Germany.
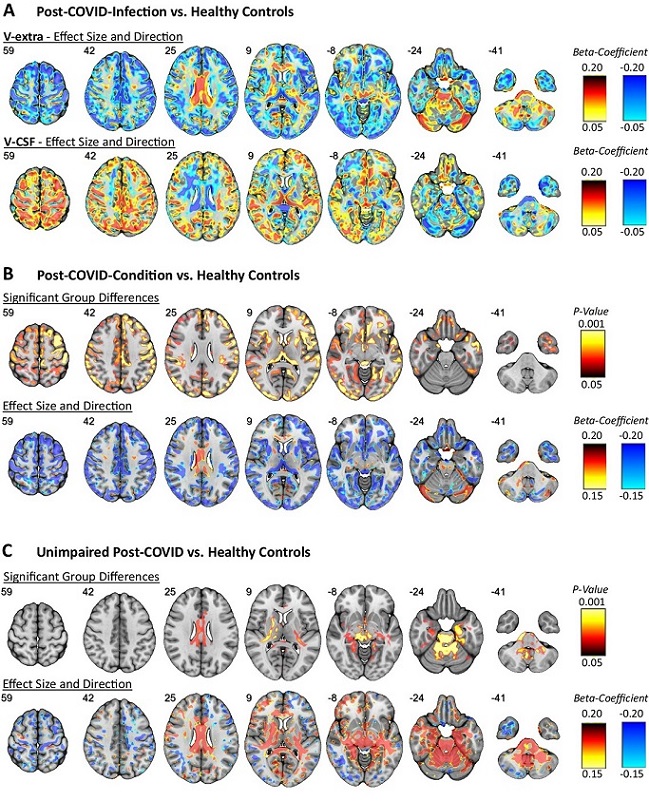
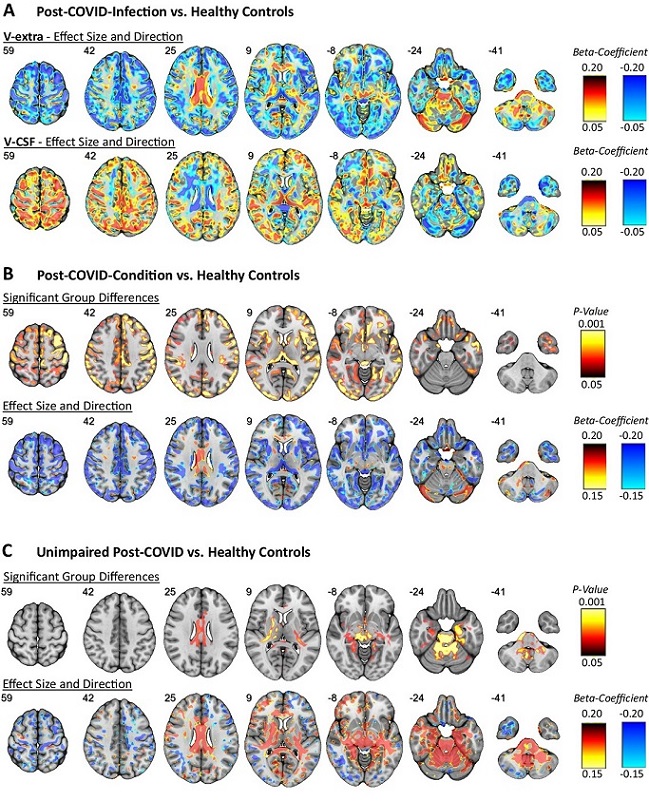 Spatial distribution and direction of microstructural changes after COVID-19
A The standardized regression coefficients of the factors V-extra and V-CSF were extracted from two-tailed linear regression models yielded by voxel-wise comparisons between all participants after COVID-19 infection (i.e., combined PCC and UPC group) and controls without a history of COVID-19 (HNC; with nuisance covariates age and sex), and were superimposed onto a T1w MRI template. Color-coding indicates the coefficient values as a measure of effect size of the factor COVID-19 (hot colors: positive effects vs. cold colors: negative effects). Results of voxel-based two-tailed linear regression models of V-extra after threshold-free cluster enhancement and FWE-correction (top row), and standardized regression coefficients derived from the same model (bottom row) between different groups: B Post-COVID-Condition (PCC) vs. Healthy Non-COVID controls (HNC), C. Unimpaired-Post-COVID participants (UPC) vs. Healthy Non-COVID controls (HNC).
Understanding Post-COVID Condition
Spatial distribution and direction of microstructural changes after COVID-19
A The standardized regression coefficients of the factors V-extra and V-CSF were extracted from two-tailed linear regression models yielded by voxel-wise comparisons between all participants after COVID-19 infection (i.e., combined PCC and UPC group) and controls without a history of COVID-19 (HNC; with nuisance covariates age and sex), and were superimposed onto a T1w MRI template. Color-coding indicates the coefficient values as a measure of effect size of the factor COVID-19 (hot colors: positive effects vs. cold colors: negative effects). Results of voxel-based two-tailed linear regression models of V-extra after threshold-free cluster enhancement and FWE-correction (top row), and standardized regression coefficients derived from the same model (bottom row) between different groups: B Post-COVID-Condition (PCC) vs. Healthy Non-COVID controls (HNC), C. Unimpaired-Post-COVID participants (UPC) vs. Healthy Non-COVID controls (HNC).
Understanding Post-COVID Condition
According to the World Health Organization (WHO), PCC is defined by a history of probable or confirmed SARS-CoV-2 infection, the presence of at least one symptom such as fatigue, shortness of breath, or cognitive dysfunction, which significantly impacts daily functioning, with symptoms persisting for at least two months and occurring three months after the initial infection. Neurological and neurocognitive symptoms are particularly prevalent in PCC, contributing significantly to the overall disease burden. Studies indicate that approximately 10-25% of COVID-19 survivors develop PCC, with a substantial impact on work-life, highlighting the urgent need for a deeper understanding of its mechanisms.
The Pathophysiology of PCC
Recent research has begun to shed light on the potential cerebral microstructural changes associated with PCC. A large longitudinal study by the UK Biobank, which analyzed pre- and post-COVID-19 brain scans, revealed increased diffusion indices within limbic regions and a reduction in cortical thickness in specific areas. These changes suggest a shif
t in brain microstructure, potentially forming the pathophysiological basis for PCC-related symptoms. However, further research is necessary to establish definitive biomarkers and understand the full extent of these alterations.
Study Overview
To investigate the cerebral microstructural changes in PCC, a team of researchers employed multi-compartment diffusion microstructure imaging (DMI). This advanced imaging technique is based on multi-shell diffusion protocols and can detect subtle changes within the brain's meso-/microstructure by segregating different anatomical compartments based on their diffusion properties. The study involved a comparative analysis of patients with PCC, healthy controls, and individuals who contracted COVID-19 but did not develop long-term symptoms.
Key Findings
The study cohort included 89 patients diagnosed with PCC, 38 individuals who recovered from COVID-19 without long-term symptoms (Unimpaired Post-COVID group, UPC), and healthy controls. The PCC group reported a high prevalence of symptoms such as impaired attention and memory, fatigue, reduced multi-tasking ability, word-finding difficulties, and olfactory dysfunction. Notably, a significant proportion of these patients were unable to work or had to reduce their workload due to their symptoms.
MRI and Cortical Morphometry
Conventional MRI and cortical morphometric analysis revealed no significant global or cortical atrophy in either the PCC or UPC groups. However, DMI parameters indicated significant microstructural changes in the brain. The PCC group exhibited a reduction in the extra-neurite volume (V-extra) and an increase in the cerebrospinal fluid volume (V-CSF) within the gray matter. These changes suggest a shift in volume from neuronal compartments to free fluid, associated with the severity of the initial infection.
Spatial Distribution of Microstructural Changes
Voxel-wise comparisons of DMI parameters highlighted distinct patterns of microstructural alterations. In the PCC group, reduced V-extra was observed in neocortical gray matter, the thalamus, and other regions, while increased V-extra was present in the corpus callosum, internal capsule, cerebellum, and brainstem. These findings indicate that different brain regions are differentially affected by PCC, with the PCC group showing more pronounced changes in cortical regions and the UPC group exhibiting more significant alterations in infratentorial areas.
Correlation with Clinical Symptoms
The study found significant correlations between specific microstructural changes and PCC-related symptoms. Reduced V-extra within the thalamus and mesiotemporal regions was associated with impaired cognitive performance. Olfactory dysfunction correlated with reduced V-extra in orbitofrontal and mesiotemporal regions, the thalamus, and cerebellum. Fatigue was linked to reduced V-extra in a network involving aminergic brainstem nuclei, autonomic hubs, and other structures.
Discussion
The findings from this study provide valuable insights into the cerebral microstructural alterations associated with PCC. The observed shift in volume from neuronal compartments to free fluid suggests a potential mechanism involving cellular shrinkage or degeneration. Interestingly, despite the significant microstructural changes, conventional MRI did not reveal any evidence of global or cortical atrophy. This discrepancy highlights the sensitivity of DMI in detecting subtle changes that may underlie PCC symptoms.
The correlation between microstructural changes and clinical symptoms underscores the importance of specific brain networks in the manifestation of PCC. For instance, the involvement of the thalamus and mesiotemporal regions in cognitive impairment aligns with their known roles in memory and visuospatial processing. Similarly, the orbitofrontal cortex and limbic structures are crucial for olfactory processing and emotional modulation, explaining their association with olfactory dysfunction.
Conclusion
This study advances our understanding of the cerebral microstructural changes in PCC and their relationship with cognitive impairment, olfactory dysfunction, and fatigue. By employing advanced imaging techniques, the researchers were able to identify distinct patterns of microstructural alterations and their clinical correlates. These findings pave the way for future research to establish definitive biomarkers and develop targeted interventions for PCC. As the global community continues to grapple with the long-term effects of COVID-19, studies like this are crucial for mitigating the impact of PCC on individuals' lives and overall public health.
The study findings were published in the peer reviewed journal: Nature Communications.
https://www.nature.com/articles/s41467-024-48651-0
For the latest
COVID-19 News, keep on logging to Thailand Medical News.