Cancer Genes That Promote Metastasis Identified, Paving The Way For Therapeutics To Prevent Cancer Spread
Source: Thailand Medical News Jan 16, 2020 6 years, 1 month, 1 week, 4 days, 9 hours, 24 minutes ago
Two
cancer-promoting
genes MYC and
TWIST1 co-opt immune system cells to enable
cancer cells to spread, but blocking a key step in this process can help prevent the disease from developing.
These research findings, published today in
eLife, may help clinicians to identify
cancer patients at risk of
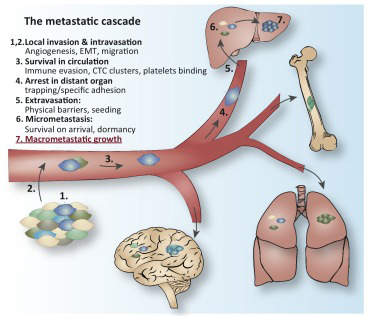
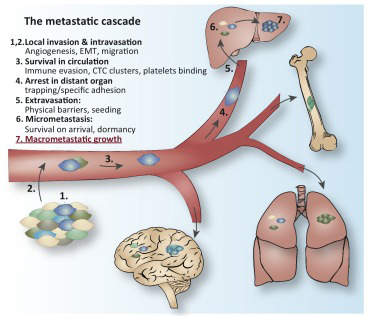
metastasis, a process where
cancer cells spread to other parts of the body. They may also inform the development of new strategies to prevent or treat
metastasis.
Lead author Dr Renumathy Dhanasekaran, a Ph.D. student in the Division of Gastroenterology and Hepatology at Stanford University, California explained to
Thailand Medical News, "Most
cancer-related deaths are caused by
metastasis, but there are currently no treatments available to stop it. The main goal of our research is to understand how
cancer-causing
genes enable
metastasis and use that information to identify targeted therapies that may prevent it."
Dr Dhanasekaran and her colleagues genetically engineered mice to express both
MYC and
TWIST1 and found that these two major
cancer-promoting
genes led to
metastases. They also saw that the
cancer cells produced inflammation-promoting molecules Ccl2 and Il13, which attract immune cells called macrophages and make them more tumour-cell friendly. This makes it easier for the
cancer cells to migrate to new areas of the body.
The research team next showed that exposing mice with liver
cancer caused by
MYC alone to Ccl2 and Il13 causes
metastasis. But blocking this specific combination of cytokines appeared to hinder the process.
To confirm if the two
genes also contributed to
metastases in humans, the scientists analysed 10,000 samples of tumours collected from humans with 33 different types of
cancer. They found that patients with
MYC and
TWIST1 were less likely to survive, produced more Ccl2 and Il13, and had more macrophages in their tumours.
Senior author Dr Dean Felsher, Ph.D., Professor in the Division of Oncology at Stanford University added, "Interestingly,
MYC and
TWIST1 have previously been shown to cooperate in a positive way to modulate inflammation during embryonic development. These microenvironment changes are needed to enable mesodermal cells to migrate to their destination. But in multiple human
cancers, both
MYC and
TWIST1 are over-expressed, and we suggest that they in turn cause tumour invasion by 'hijacking'
this embryonic cell migration program."
Lastly, the research team monitored Ccl2 and Il13 levels in 25 patients with liver
cancer and 10 control patients with cirrhosis. They found that only the patients with liver
cancer had elevated levels of the two molecules and, of this group, those with higher levels of Il13 were more likely to have aggressive tumours.
Dr Felsher concludes, "These results suggest that patients with more aggressive
cancers will likely have higher levels of Ccl2 and Il13 cytokines in their blood. Testing for these molecules in future could help identify those who may benefit from combination therapies that target them."
Reference: Renumathy Dhanasekaran et al, MYC and Twist1 cooperate to drive metastasis by eliciting crosstalk between cancer and innate immunity, eLife (2020). DOI: 10.7554/eLife.50731